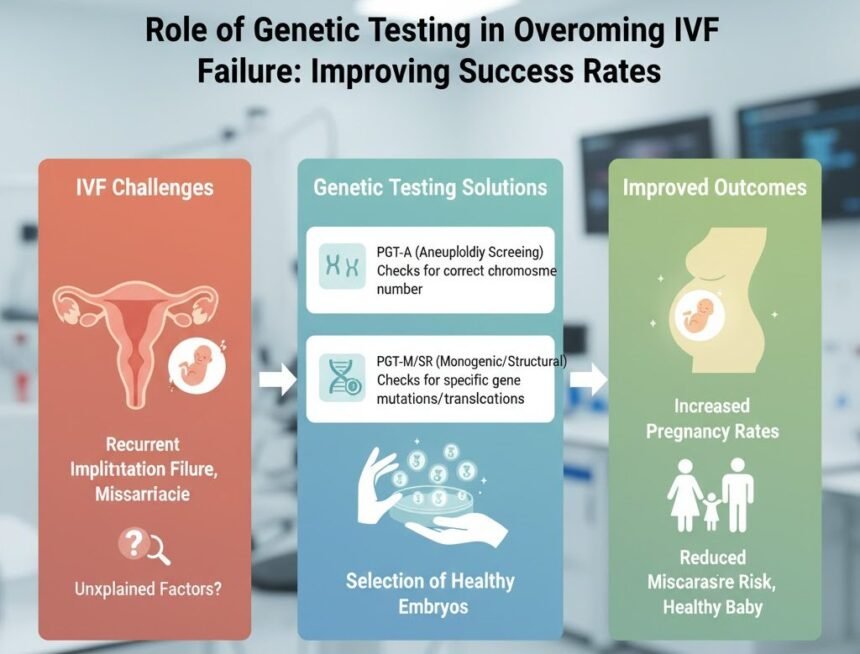
Overcoming IVF failure often involves testing for hidden conditions, such as endometriosis and genetic disorders. These conditions can affect uterine health, implantation, and embryo development. Genetic testing enables doctors to identify potential mutations and provides information that may inform decisions about a child’s health. Here are a few roles of gene testing in overcoming failure during IVF treatment:
Identifying Genetic Disorders
- Fertility specialists may perform pre-implantation genetic testing for aneuploidy (PGT-A) to detect abnormal chromosome numbers, and they can also utilize pre-implantation genetic testing for monogenic conditions (PGT-M) to assess heritable conditions. Other tests include karyotyping, which evaluates chromosomal structure for changes that might influence IVF outcomes. These procedures provide detailed information about the embryos before transfer.
- Genetic testing helps identify embryos with abnormalities early, so transfers can focus on those most likely to develop normally. Embryos with detected issues are usually set aside, while unaffected embryos may continue through the process, which can help reduce the chances of IVF failure. Doctors may also recommend alternatives, such as donor eggs or sperm, when needed. Testing allows healthcare providers to offer guidance that may support embryo quality and inform future IVF strategies.
Authoritative sources: American Society for Reproductive Medicine, CDC – Assisted Reproductive Technology, NIH Genetics Home Reference.
Selecting High-Quality Embryos
- Genetic testing provides measurable biological indicators that can inform the selection of embryos. PGT-A screens give fertility specialists data on chromosome number and structure, helping them focus on euploid embryos. These embryos often show more consistent development patterns, which can support smoother transfer planning. Testing adds objectivity to the selection process, moving beyond traditional visual assessments.
- Refining selection methods may reduce the number of cycles required for transfers, thereby streamlining timelines for patients. Clinics also offer options, such as frozen embryo transfers, to provide flexibility in treatment scheduling. Combining genetic assessments with conventional grading offers additional insights and supports overall IVF workflow efficiency.
- Embryo development can be tracked using standard chromosomal profiles alongside laboratory techniques, such as blastocyst culture and time-lapse imaging. This combination allows specialists to adjust protocols based on observed trends. By analyzing data across multiple cycles, clinics can refine processes and improve planning for future treatments.
Reference: European Society of Human Reproduction and Embryology (ESHRE).
Enhancing Treatment Strategies
- Genetic testing provides information that can guide IVF planning. Test results may influence medication timing, egg retrieval scheduling, and the choice between fresh or frozen embryo transfers. Once viable embryos are identified, specialists can create a more structured timeline for current and future treatment cycles. This process supports coordinated planning while maintaining flexibility for patients.
- Fertility teams may preserve other viable embryos while waiting for optimal conditions for transfer. Testing allows doctors to adjust techniques, such as assisted hatching, and refine individualized treatment strategies. Customization helps align IVF procedures with each patient’s biological profile, creating a tailored approach to care.
- For families with known inherited conditions, genetic testing helps identify embryos that carry potential mutations. These embryos may be excluded from transfer, which can influence family planning decisions. Testing data also provides insights that allow specialists to make informed adjustments and reduce the chances of IVF failure.
Reference: National Institute of Child Health and Human Development.
Improving Long-Term Planning
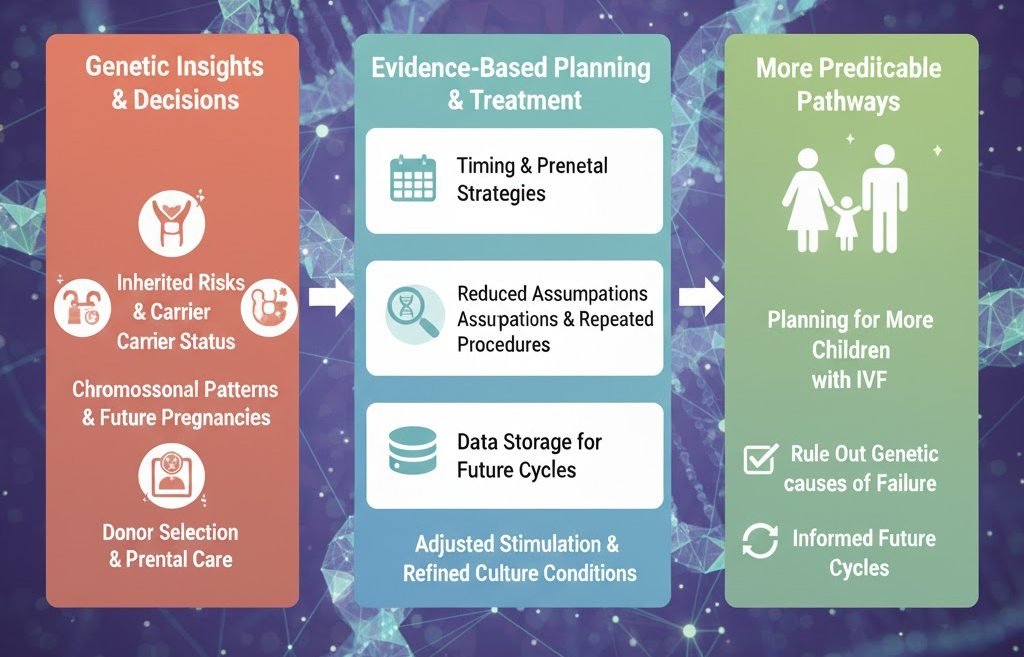
- Genetic testing supports decisions beyond the current IVF cycle. Results offer insight into inherited risks, carrier statuses, and chromosomal patterns that may affect future pregnancies and treatment. Doctors also use the information to help couples plan aspects, such as timing, donor selection, and prenatal care strategies.
- Evidence-based planning reduces assumptions that may lead to repeated procedures. The data from pre-implantation and prenatal testing are stored for future reference and use in subsequent treatment cycles. Clinics may use this record to adjust stimulation procedures or refine embryo culture conditions, improving selection criteria over time.
- By incorporating genetic insights into long-term reproductive planning, doctors create more predictable pathways for future pregnancies. This insight is helpful when planning to have more children with the help of IVF treatment. Testing also helps rule out genetic issues as the underlying cause of failed IVF.
Reference: Mayo Clinic – IVF and Genetic Testing.
Learn More About Overcoming IVF Failure
- Genetic issues are often among the primary contributors to implantation failure and early pregnancy loss. Other potential factors include endometriosis, chronic bacterial infections, and various conditions that influence uterine health and function. Understanding these factors can provide valuable insight into reproductive challenges and treatment planning. Consider getting tested today to start learning more about IVF failure, possible causes, and prevention strategies.
Conclusion
Genetic testing plays a crucial role in identifying underlying issues that may contribute to IVF failure. By detecting chromosomal abnormalities, refining embryo selection, and informing treatment strategies, genetic insights help fertility specialists develop more personalized and effective IVF plans. This proactive approach can improve implantation rates, reduce failed cycles, and support healthier pregnancies.
Disclaimer: This information is for educational purposes only and is not a substitute for professional medical advice. Always consult with a qualified fertility specialist or reproductive endocrinologist to determine the most appropriate testing and treatment options for your individual circumstances.