Pain in the big toe joint (medically, the first metatarsophalangeal or MTP joint) can be surprisingly debilitating. This joint is crucial for balance, walking, and pushing off the ground, meaning that even mild stiffness or pain can impact your mobility and quality of life. Whether you’re experiencing the deep ache of arthritis or the sharp tenderness of a flare-up, the underlying issue is often wear, tear, or inflammation that restricts the joint’s smooth function. The goal of this guide is to provide you with clear, practical steps for reducing inflammation and restoring comfortable movement.
What Causes Non-Traumatic Big Toe Joint Pain?
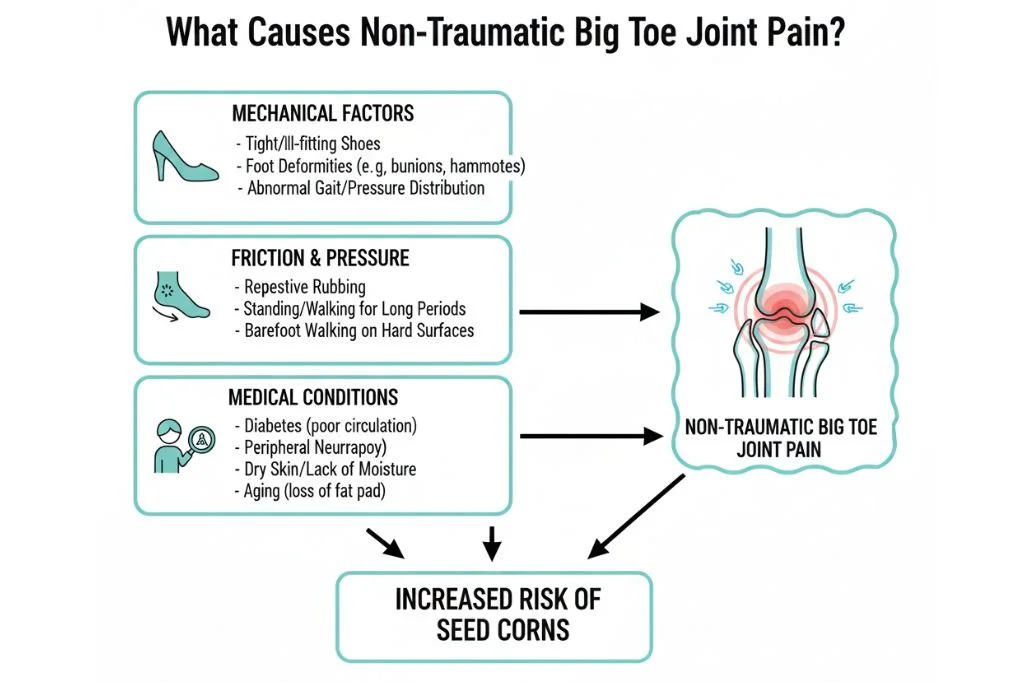
The most common causes of persistent, non-injury related pain in the big toe joint are forms of arthritis or mechanical dysfunction that limit the joint’s range of motion.
Common Diagnoses
- Hallux Rigidus/Limitus: This is a progressive condition where the joint cartilage wears down, leading to stiffness (rigidus) or limited movement (limitus). Bony spurs often form, making movement painful.
- Gout: A specific type of inflammatory arthritis caused by a buildup of uric acid crystals in the joint. It typically causes sudden, severe, hot, and intensely painful attacks.
- Osteoarthritis: General “wear and tear” arthritis, commonly affecting the MTP joint over time due to high mechanical stress.
Primary Pain Triggers
Identifying and avoiding triggers can significantly reduce daily pain.
- Footwear: High heels, shoes with a narrow toe box, or shoes with very flexible soles (requiring excessive MTP joint movement).
- High-Impact Activities: Running, jumping, or sports that involve repeated push-off from the forefoot.
- Excess Weight: Places higher load stress on all joints, particularly the weight-bearing joints of the foot.
- Sudden Dietary Changes (Gout): Excessive consumption of purine-rich foods (red meat, seafood, alcohol).
Immediate Relief and Mechanical Support
When the joint is inflamed, the first priority is to reduce the swelling and restrict painful movement.
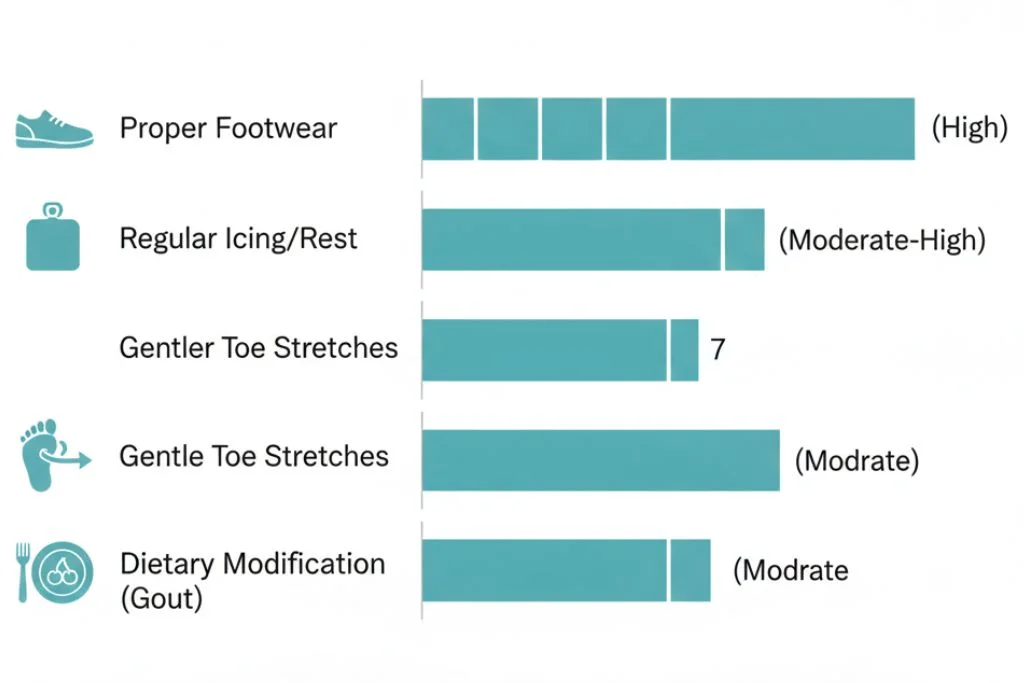
1. Simple R.I.C.E. Protocol (Step-by-Step for Feet)
The R.I.C.E. method remains the cornerstone of acute inflammation management.
- Step 1: Rest. Limit walking and standing. If pain is severe (e.g., during a gout flare), stay off the foot completely.
- Step 2: Ice. Apply an ice pack (wrapped in a thin towel) to the top of the joint for 15–20 minutes. Do this 3–4 times per day.
- Step 3: Compression. Use a mild compression bandage or sleeve around the foot and ankle, ensuring it’s snug but not tight enough to cut off circulation.
- Step 4: Elevation. Prop the foot up so the toe joint is above the level of the heart to encourage fluid drainage.
2. Strategic Footwear Modification
The right shoe minimizes painful motion and pressure. Look for shoes that are stiff in the sole.
Key Features to Look For:
| Feature | Benefit for Big Toe Pain |
| Rocker Bottom Sole | Limits the painful flexing of the MTP joint during the push-off phase of walking. |
| Wide, Deep Toe Box | Prevents lateral compression and rubbing on bony spurs. |
| Stiff Shank | Prevents the entire forefoot from bending excessively. |
| Low Heel | Avoids shifting body weight onto the forefoot. |
Proactive Prevention: Diet and Movement
For long-term joint health, particularly in cases of osteoarthritis or managing gout, lifestyle changes are essential.
Role of Specific Nutrition (Gout Focus)
Dietary management is particularly important for those managing recurrent gout flare-ups.
| Food Group | Gout Risk Status |
| High Purine (Red Meat, Organ Meats, Shellfish, Beer) | High Risk (Limit Consumption) |
| Moderate Purine (Poultry, Beans, Oats) | Moderate Risk (Consume in Moderation) |
| Low Purine (Fruits, Vegetables, Dairy, Whole Grains) | Low Risk (Encouraged) |
Anti-Inflammatory Food List (Helpful for Osteoarthritis):
- Omega-3 Sources: Fatty fish (salmon, mackerel), flaxseeds, walnuts.
- Antioxidants: Berries, dark leafy greens (spinach, kale), turmeric.
- Cherries: Some evidence suggests they may lower uric acid levels and reduce gout attacks.
- Water: Maintaining high fluid intake helps flush uric acid.
3. Gentle Range-of-Motion Exercises
Maintaining flexibility around the joint can prevent further stiffening (rigidus), provided the joint is not in an acute flare.
Effectiveness of Home Management Techniques:
Instruction: Perform these slowly, stopping immediately if they cause sharp pain.
- Toe Flex and Extend: While seated, gently bend the big toe up (extension) toward the ceiling, holding for 5 seconds, then down (flexion) toward the floor, holding for 5 seconds. Repeat 10 times.
- Ankle Circles: Rotate the ankle and foot gently 10 times clockwise and 10 times counter-clockwise. This warms up the entire foot structure without straining the MTP joint.
When to See a Doctor
While self-care is effective for mild, occasional pain, certain symptoms require professional evaluation by a podiatrist or orthopedist.
- Intense, Sudden Swelling: If the joint becomes instantly hot, red, and swollen, preventing all weight-bearing (classic gout or acute infection).
- Persistent Limping: Pain that severely restricts your ability to walk or forces a change in your gait.
- Bilateral Involvement: Pain that suddenly starts affecting both big toe joints simultaneously.
- Non-Response to Treatment: If the pain does not improve after 1–2 weeks of consistent R.I.C.E. and appropriate footwear changes.
- Fever or Chills: Pain accompanied by systemic signs of infection.
Improvement Timeline
The timeline for improvement depends heavily on the underlying diagnosis and adherence to the plan.
| Intervention Stage | Expected Improvement |
| Acute Gout Flare (Medication) | 2–5 days (Significant pain reduction) |
| Managing Osteoarthritis (Footwear/Icing) | 2–4 weeks (Reduction in daily pain frequency/severity) |
| Achieving Functional Stability | 3–6 months (Long-term pain management and increased mobility) |
Final Advice
Your big toe joint is a complex, hard-working structure. If it signals distress, listen carefully. Managing persistent pain requires patience and dedication to mechanical support. Prioritize shoes that work for your joint, not against it, and remain consistent with gentle mobility work. By respecting the joint’s limitations and controlling inflammation, you can maintain function and significantly enhance your daily comfort.
Medical Disclaimer
This article is intended for informational and educational purposes only and does not constitute medical advice, diagnosis, or treatment. It is not a substitute for professional medical or orthopedic care. Always consult with a qualified healthcare provider regarding any persistent joint pain, swelling, or before making any changes to your medication or treatment plan.
References
- Coughlin, M. J., et al. (2022). Hallux Rigidus: A comprehensive review of pathophysiology and treatment. Journal of Orthopaedic Surgery and Research.
- Dalbeth, N., et al. (2023). Diet and gout: a systematic review of the evidence and practice recommendations. Arthritis Research & Therapy.
- American Academy of Orthopaedic Surgeons (AAOS). (2024). Foot and Ankle Pain: First Metatarsophalangeal Joint Disorders.
- Rome, K. (2021). The role of footwear in the management of foot and ankle musculoskeletal disorders. The Foot.

