If you wake up around 2 AM with a pounding headache and slight chills, it is easy to pop open the cabinet and grab a bottle of Ibuprofen you keep for just such emergencies. You take a couple of tablets with tap water and go back to bed. By morning, you feel fine enough to go to work.
We all self-medicate without even thinking about it. According to a 2023 study published in the National Library of Science, between 11% to 92% of people self-medicate in different parts of the world, of course, without consulting a health professional.
It’s fast, it’s convenient, and honestly, it’s tempting to handle things yourself. But is self-medication safe?
When you into your cache of leftover prescriptions, are you helping yourself or just making things worse?
Let’s find out.
What Is Self-Medication?
Self-medication means using medicines, herbal remedies, or supplements to treat yourself for illness without first consulting with a healthcare professional.
Whether it’s reaching out for leftover ibuprofen, taking old antibiotics you found in the medicine cabinet for your scratchy throat, or popping miracle herbal pills you bought over the internet, it’s all the same thing.
Even the vitamins, over-the-counter cough syrups, and sleeping pills you’ve been taking for the past thirty years without issues fall into this category.
So, is it harmful? It depends. If you get a mild paper cut, you grab a Band-Aid. That’s a form of self-medication. If a headache suddenly shows up and you take a regular dose of paracetamol, that’s usually fine too.
The problem is when we start treating severe symptoms like they’re minor or take the wrong medication for the wrong problem.
Take dehydration, for example. It can give you a pounding headache. Taking a pain reliever without drinking lots of water will not address the real cause of the headache. You’re only silencing the message your body is trying to send, which can make things worse later.
Genuine Risks of Self-Medication
While it’s true that not all self-medication is harmful, it’s still a risky thing to do. Let’s look at the potential risks of cutting out the professional safety net.
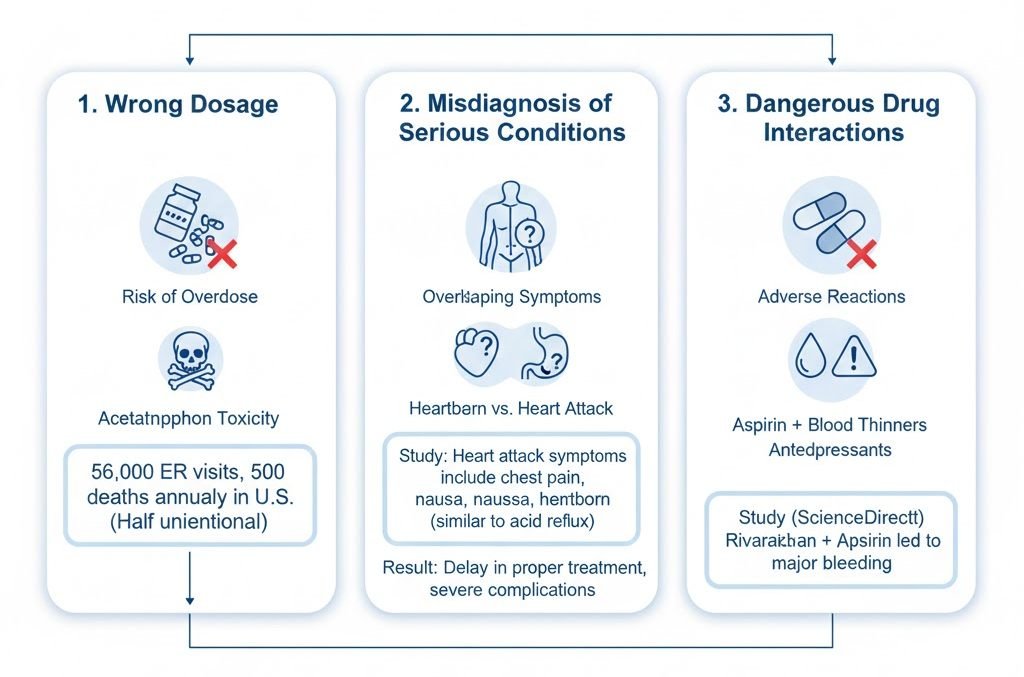
Wrong Dosage
Taking the wrong dosage is one of the big problems with self-medication. Say, you have a stubborn backache. What do you do? Take some acetaminophen. And then you take some more, risking overdose. You probably think that doubling up on the pain reliever will handle the issue faster.
But here’s what you may not know. Acetaminophen toxicity is responsible for about 56,000 emergency department visits and 500 deaths annually in the U.S.A. And guess what? Around half of those cases are unintentional.
People don’t realise they’re taking too much of it, especially when they take products like cold medicines and prescription painkillers that contain acetaminophen.
Misdiagnosis of Serious Conditions
Another terrifying one is misdiagnosis. That stomachache you told Mary in HR to take Pepto Bismol for might actually be a sign of a gallbladder issue. That persistent heartburn you’re treating with over-the-counter antacid? How are you sure it’s not actually a heart issue?
A 2023 study on Acute Myocardial Infarction published on Research Gate breaks down this scenario succinctly: The classic symptoms of a heart attack include chest pain, nausea, vomiting, and heartburn. People with gastroesophageal disease or acid reflux also experience the same.
Seeing as these symptoms overlap, you might be treating ordinary heartburn, not knowing it’s something much worse.
The scenarios are endless. Unfortunately, when you guess wrong about what’s going on in your body and try to treat it yourself, you’re not saving time. You’re gambling. That gamble comes at a steep price.
Dangerous Drug Interactions
You know how we usually take different medicines for different reasons, usually at the same time or close together? Turns out that’s not a good thing. Some of these medicines interact with each other, making them ineffective or causing adverse reactions.
Take aspirin, for example. It’s not advisable to take it with a blood thinner. This combination can put you at risk of severe bleeding. But not many people know this.
In fact, a registry study of 1,467 patients that took place over a period of 18 months, and recently published on ScienceDirect, found that people taking rivaroxaban in addition to aspirin suffered major bleeding. Those on warfarin plus aspirin mainly experienced only minor bleeding.
Rivaroxaban and Warfarin are types of blood thinners.
Cold medicine and antidepressants are another combination that can be dangerous.
People have ended up in the ER simply because they didn’t know that certain medicines shouldn’t be taken together.
When Is it Okay to Self-Medicate?
So, does this mean that your medicine cabinet is now a no-go area? Not exactly. There are times when you have no option but to self-medicate.
You can’t be having a blinding headache, for example, and not do anything about it until you see the doctor. In this type of situation, your first goal is to bring the ache down.
The same thing applies to a sudden scratchy throat. While waiting for a diagnosis and expert help, a lozenge can provide mild relief. That’s where self-medication makes sense.
In addition to treating or managing ailments, vitamins are also okay. In fact, medical experts recommend a daily dose of vitamins A, D, E, K, and C, as well as the B vitamins. They also recommend iron, zinc, calcium, magnesium, and omega-3 fatty acids. You’ll usually get these vitamins in your daily diet, but you’re also fine to take them as supplements.
As you can see, these examples fall under the minor ailments category. Things like mild cold, period cramps, simple cuts, indigestion, and so on. These are the symptoms you can treat on your own with OTC drugs.
That said, you must know a few best practices for self-medication to help keep everything safe and risk-free.
These are the golden rules of safe at-home treatments:
- Read the Label: This one should go without saying, but it’s essential we reiterate it — read the label of every medicine before taking it, always. The label will tell you the recommended dosage, any possible interactions with other drugs, and, more importantly, the expiry date. Follow the instructions that concern you religiously.
- Check for Interactions: If you come across a new brand of the medicine you typically take, don’t be in a hurry to try it. First, check that it doesn’t interact negatively with anything you already have in your cabinet. It won’t take more than a few minutes to double-check these details with your pharmacist.
- Don’t Over-Rely: Possibly the most important of them all, don’t over-rely on your medicine cabinet. A simple headache that comes back every afternoon is not simple. It’s definitely a sign of something bigger. Remember the popular quote, “if symptoms persist after three days, consult your doctor”; it’s not just a nice marketing copy. It’s advice you should stick to.
Role of Healthcare Professionals
So, what happens when you have a significant health challenge, and you’ve got a potential solution in your medicine cabinet? The answer is simple: don’t take it.
We’ve already covered this, but it’s worth repeating. How can you be sure that the symptoms you’re experiencing are not signs of something else? For example, a severe headache can be caused by being short on sleep, dehydrated, or stressed. It could also be a sign of sinus or eye infection, or that you’ve got the flu. So, which is it?
This is precisely why we have healthcare professionals. These don’t just hand out prescriptions and send you home. They first assess your symptoms and check your medical history. Then guide you towards the best and safest options.
A registered nurse, for example, is extensively trained to administer medicine safely. They know how different drugs interact and what to look for before making any recommendation. You don’t have this type of knowledge, no matter how many medical blogs you’ve read.
And for nurses who want to take things a step further, RN-to-NP programs online help them build stronger clinical skills as nurse practitioners. They can diagnose, prescribe, and provide more comprehensive patient care.
Wilkes University explains that these programs focus on advanced clinical skills needed to improve patient outcomes. In other words, they understand complex health conditions, drug pharmacokinetics, and, most importantly, you, the whole patient.
So, apart from the minor ailments we mentioned initially, your best bet when you fall sick is to see a health professional. They can look at your whole picture — your health history, any meds you’re currently taking, your lifestyle — and give you expert guidance that a Google search, ChatGPT, or a bottle label simply cannot.
When to Seek Professional Help
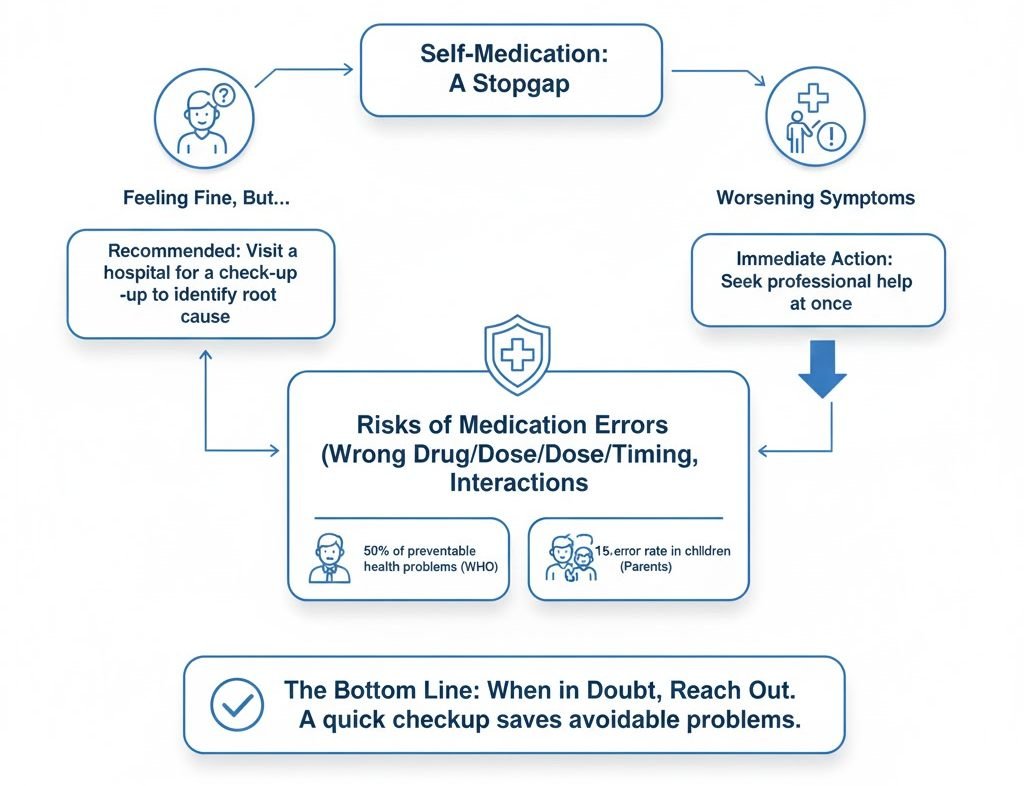
No matter how effective you think the drugs you’re taking are, self-medication is actually just a stopgap. Even if you feel fine, it makes sense to visit the hospital and check out what went wrong in the first place.
But if you’re not getting any better or your situation is worsening despite the medicine you’re taking, seek professional help at once. Maybe you’re getting things wrong. The World Health Organisation (WHO) reports that 50% of preventable health problems can be traced to the wrong drug, wrong dose, wrong timing, or dangerous interactions.
And it’s not just adults only. A study of 730 parents recently published in the Journal of Pediatric Nursing found a 15% medication-error rate when parents self-medicate their children at home. Mostly, they miss the recommended drug dose.
These mistakes happen more often than most people realise, and they can lead to serious complications if ignored.
The bottom line? When in doubt, reach out. A quick checkup can save you from a long list of avoidable problems.
Conclusion
Self-medication isn’t inherently harmful. When used thoughtfully, it can help you manage minor ailments until you can see a doctor. Just don’t make a habit of it.
Safe medication isn’t about not taking another aspirin without a doctor’s say-so. It’s about knowing your limits, paying attention to what your body is telling you, and knowing when it’s better to let a healthcare professional step in.
Disclaimer
The information in this article is for educational and general awareness purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Do not rely on self-medication for serious or persistent symptoms. Always consult a licensed healthcare provider before starting, stopping, or combining any medications, supplements, or treatments. If you experience worsening symptoms or signs of a medical emergency, seek medical help immediately.
References
Centers for Disease Control and Prevention (CDC).
- Acetaminophen: Drug Safety Communication.
- Discusses risks of overdose and safe dosing practices.
National Institutes of Health (NIH) – MedlinePlus.
- Drug Interactions Overview.
- Explains how medications can interact and why mixing them without guidance is risky.
World Health Organization (WHO).
- The Pursuit of Responsible Self-Medication.
- Addresses global mistakes in self-medication, dosing errors, and preventable adverse effects.
National Center for Complementary and Integrative Health (NCCIH).
- Herbal Medicines and Supplements: Safety Considerations.
- Highlights risks of supplements and herb–drug interactions.
Journal of Pediatric Nursing (Elsevier).
- Parent medication-administration error rates study (730 participants).
- Shows how dosing mistakes happen frequently at home.
American Heart Association (AHA).
- Heart Attack Symptoms and Diagnosis.
- Explains overlap between heartburn and cardiac symptoms.
U.S. Food and Drug Administration (FDA).
- Using Over-the-Counter Medicines Safely.
- Provides guidelines for correct dosing, label reading, and avoiding interactions.

