It’s common for many individuals to notice variations in skin tone across different parts of their body, and the intimate areas are no exception. The skin around the vulva and inner thighs can naturally be darker due to various factors like genetics, hormonal changes, friction, and age. While this is a completely normal physiological phenomenon, some individuals may feel self-conscious or seek aesthetic changes for personal reasons. Understanding the available options, their safety, and potential outcomes is crucial for making informed decisions about “vaginal whitening” or intimate area lightening.
Science Behind Skin Pigmentation in Intimate Areas
The color of our skin is primarily determined by melanin, a pigment produced by cells called melanocytes. Various factors can influence melanin production, leading to hyperpigmentation in sensitive regions.
Factors Contributing to Darker Skin Tone
- Genetics: Just like hair or eye color, skin pigmentation patterns are inherited. Some individuals are naturally predisposed to darker intimate areas.
- Hormonal Fluctuations: Puberty, pregnancy, hormonal birth control, and menopause can all lead to increased melanin production, causing darkening.
- Friction and Chafing: Constant rubbing from tight clothing, exercise, or even skin-on-skin contact can irritate the skin, triggering melanocytes to produce more pigment as a protective response.
- Aging: As we age, skin can undergo various changes, including alterations in pigmentation.
- Inflammation: Conditions like folliculitis (inflammation of hair follicles) or chronic irritation from shaving or waxing can cause post-inflammatory hyperpigmentation.
- Sun Exposure: While often covered, prolonged exposure to UV rays can also contribute to darkening, especially in areas not always protected.
How “Whitening” or Lightening Works
Most methods aim to either reduce melanin production or gently exfoliate darker surface skin cells.
- Melanin Inhibition: Ingredients that block the enzyme tyrosinase (essential for melanin production) can lighten existing pigmentation and prevent new darkening.
- Exfoliation: Gently removing the top layers of skin encourages the growth of new, lighter-pigmented skin cells.
A Practical Look at Vaginal Whitening Methods
Various approaches exist, ranging from topical creams to professional procedures. Each has its own mechanism, efficacy, and safety profile.
| Method Category | Common Ingredients/Techniques | Mechanism of Action | Considerations |
| Topical Creams | Hydroquinone (prescription), Kojic Acid, Alpha Arbutin, Vitamin C, Niacinamide, Retinoids | Inhibits melanin production; promotes exfoliation | Requires consistent use; patch test essential; prescription for stronger agents. |
| Chemical Peels | Alpha Hydroxy Acids (AHAs), Trichloroacetic Acid (TCA) | Controlled exfoliation of outer skin layers | Performed by professionals; varying strengths; downtime. |
| Laser Therapy | Fractional Lasers (e.g., CO2), Q-switched Lasers | Targets melanin; stimulates cell turnover | Professional procedure; multiple sessions; recovery time; potential risks. |
| Microdermabrasion | Mechanical exfoliation with fine crystals | Removes superficial dead skin cells | Less invasive; multiple sessions needed; temporary results. |
Treatment: What to Expect
Regardless of the chosen method, a careful approach, especially in sensitive areas, is paramount.
General Step-by-Step for Professional Treatments
This applies to chemical peels and laser therapy.
- Initial Consultation: A thorough discussion with a dermatologist or aesthetic physician to assess suitability, discuss expectations, risks, and determine the best approach.
- Skin Preparation: May involve using topical products for a few weeks prior to prime the skin and enhance results.
- Procedure Session: The chosen peel or laser treatment is carefully applied to the targeted areas by a trained professional.
- Post-Procedure Care: Strict adherence to aftercare instructions, including gentle cleansing, moisturizing, and avoiding irritants or friction.
- Follow-up Sessions: Multiple sessions are often required, typically spaced weeks apart.
- Maintenance: Ongoing care and potentially touch-up treatments to sustain results.
Important Considerations for All Methods
- Patch Testing: Always perform a patch test with any new topical product to check for sensitivity or allergic reactions.
- Avoid Self-Treating with Strong Agents: Over-the-counter products are generally milder. Prescription-strength treatments should ONLY be used under medical supervision.
- Patience: Results are typically gradual and require consistent application or multiple sessions.
- Hygiene: Maintain excellent hygiene to prevent irritation or infection, especially post-procedure.
Long-Term Safety and Expected Outcomes
Safety is paramount, especially when treating sensitive areas. Unrealistic expectations can lead to dissatisfaction.
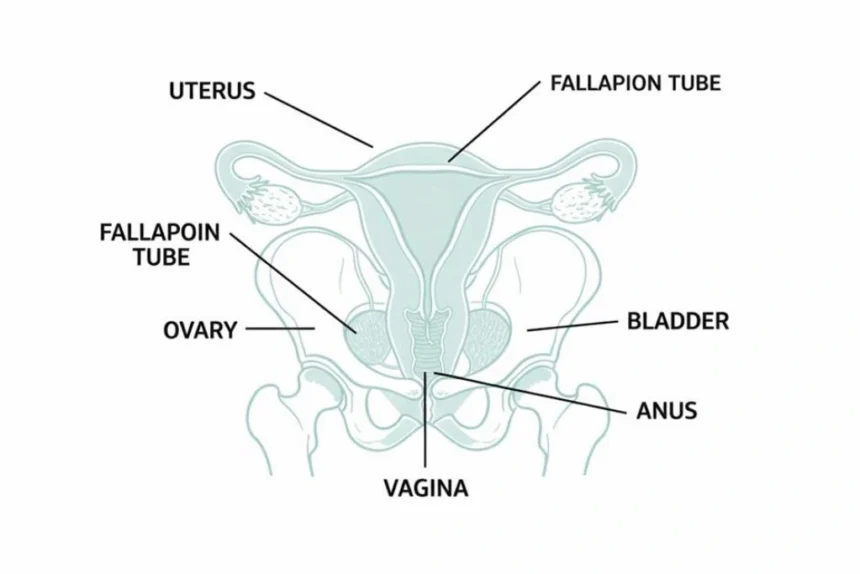
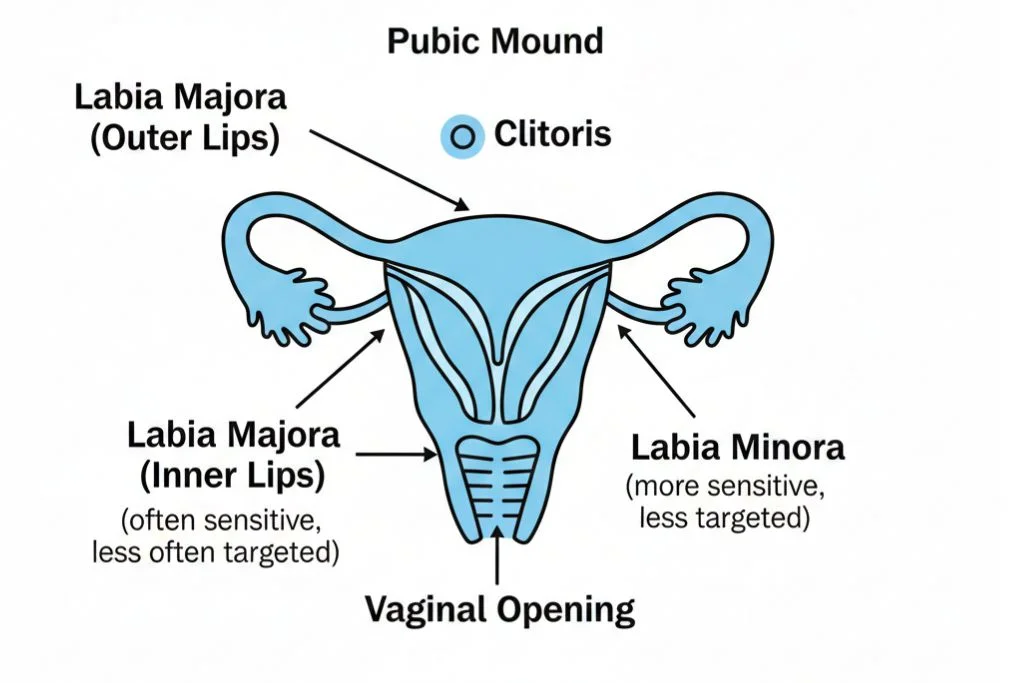
Diagram: Anatomy of the Vulva (External Genitalia)
It’s important to understand the specific areas commonly targeted for lightening.
Potential Risks and Side Effects
- Irritation & Inflammation: Redness, itching, burning, swelling.
- Allergic Reactions: Rash, hives, severe itching.
- Post-Inflammatory Hyperpigmentation (PIH): Ironically, aggressive or improper treatment can cause further darkening.
- Hypopigmentation: Permanent lightening that results in a patchy or uneven appearance.
- Scarring: A rare but serious risk with aggressive procedures.
- Infection: Risk if proper hygiene and aftercare are not followed.
- Unrealistic Expectations: Complete “whitening” to an unnaturally light shade is often not achievable or advisable. The goal is typically a more even and slightly lighter tone.
Effectiveness and Client Satisfaction
Results vary, and realistic expectations are key.
Graph: Client Satisfaction vs. Method
This table provides a general sense of satisfaction levels based on typical outcomes and invasiveness.
| Method Category | Typical Outcome | Satisfaction Level (General) |
| Topical Creams | Gradual, mild to moderate lightening | Moderate |
| Chemical Peels | Moderate to significant lightening | Good |
| Laser Therapy | Significant, more uniform lightening | Very Good |
| Microdermabrasion | Mild, superficial lightening, temporary | Low to Moderate |
Note: Satisfaction is highly dependent on individual expectations, skin type, and practitioner skill.
When to See a Doctor
Always consult with a healthcare professional before attempting any intimate area lightening procedure, especially if considering professional treatments or experiencing adverse reactions.
- Before Starting: Discuss your concerns with a dermatologist or gynecologist to rule out underlying medical conditions causing hyperpigmentation.
- Adverse Reactions: If you experience severe redness, burning, blistering, persistent itching, or any signs of infection (pus, fever) after using a product or undergoing a procedure.
- Uncertainty: If you are unsure which method is safe or appropriate for your skin type and desired outcome.
Improvement Timeline
| Method | Initial Visible Change | Optimal Results Timeline | Maintenance Needed |
| Topical Creams | 4-8 weeks | 3-6 months | Ongoing |
| Chemical Peels | 1-2 weeks (after first) | 2-4 months (after multiple) | Periodically |
| Laser Therapy | 2-4 weeks (after first) | 3-6 months (after multiple) | Periodically |
Final Advice
Variations in intimate skin tone are normal, and embracing your natural body is always a healthy choice. If you choose to explore “vaginal whitening,” approach it with caution, realistic expectations, and, most importantly, under the guidance of a qualified medical professional. Prioritize your health and safety above all else, ensuring any chosen method is both effective and medically sound.
Medical Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. It is not a substitute for professional medical care. The information provided should not be used for self-diagnosis or self-treatment. Always consult with a qualified dermatologist, gynecologist, or aesthetic physician regarding any skin concerns, medical conditions, or before making decisions about cosmetic procedures.
References
- Draelos, Z. D. (2010). Cosmetic Dermatology: Products and Procedures. Wiley-Blackwell.
- American Academy of Dermatology Association (AAD). Hyperpigmentation: Diagnosis and Treatment.
- Journal of Clinical and Aesthetic Dermatology. Topical Agents for the Treatment of Hyperpigmentation.
- Lasers in Surgery and Medicine. Laser Treatment of Pigmented Lesions.