Fasting has become incredibly popular, and for good reason. Taking intentional breaks from eating can help with weight management, improve your metabolism, and even support longevity. But here’s what I hear most often in my office: “How often should I actually be doing this?”
The truth is, there’s no one-size-fits-all answer. What works for your neighbor might not work for you. The key is finding a rhythm that fits your life, your health, and your goals without making you miserable.
First Things First: Not All Fasts Are Created Equal
When we talk about fasting, we need to be clear about what kind we mean. A 14-hour overnight fast (which you might already be doing without realizing it) is completely different from a multi-day water fast.
Here are the three main types I see people using successfully:
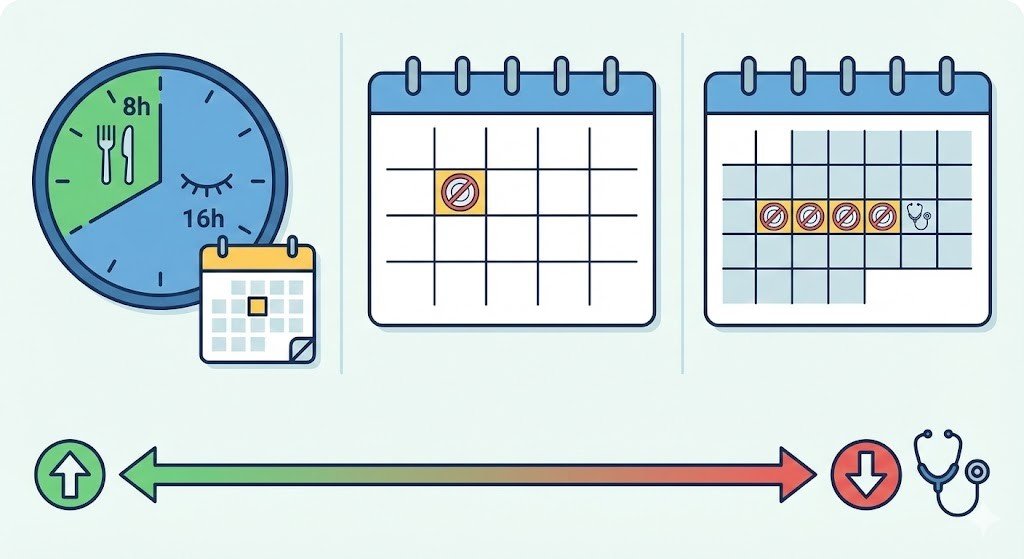
- Daily fasting (Time Restricted Eating): You eat all your meals within a shorter window each day, typically 8 hours, and fast for the remaining 16 hours.
- Weekly fasting: You do a full 24-hour fast once or twice a week. For example, you finish dinner Monday night and don’t eat again until dinner Tuesday.
- Extended fasting: These are longer fasts lasting 2 days or more. These are much more intense and need careful planning and medical oversight.
Here’s the golden rule: the longer the fast, the less often you should do it, and the more important it becomes to work with a healthcare provider.
Daily Time Restricted Eating: Best Starting Point
For most healthy people, I recommend starting here. It’s the easiest to stick with and delivers real benefits without being overly restrictive.
- What it looks like: The most popular version is 16:8. You fast for 16 hours (including sleep time) and eat during an 8-hour window. For instance, stop eating by 7 PM and don’t eat again until 11 AM the next day.
- How often: You can do this every day or most days of the week (5-7 days).
- Why it works: This approach helps your body become better at switching between burning carbohydrates and burning stored fat. It improves insulin sensitivity, which is especially helpful for managing blood sugar and weight. The best part? You’re not drastically changing what you eat, when you eat it.
Patient story: I had a pre-diabetic patient. She didn’t overhaul her entire diet. She stopped eating after 7 PM (no more late-night snacks) and pushed her breakfast to 11 AM instead of 7 AM. She still had her coffee in the morning, just black. Six months later, her fasting blood sugar had dropped significantly. Her body finally had time each night to process glucose and do repair work instead of constantly digesting food.
Pro tip: Start with a 12-hour fast (like 7 PM to 7 AM) and gradually extend it. You don’t have to jump straight to 16 hours.
Weekly 24-Hour Fasts: Stepping It Up
Once you’re comfortable with daily time-restricted eating, some people choose to add a full 24-hour fast once or twice a week.
- What it looks like: Pick one or two days a week (like Monday and Thursday). Eat dinner one evening, then don’t eat again until the next evening’s dinner.
- How often: Once or twice per week maximum. Consistency matters more than frequency.
- Why it works: A 24-hour fast depletes your stored glucose (glycogen) and pushes your body into fat-burning mode for several hours. It can help break through weight-loss plateaus and give your digestive system a real break.
Practical advice: Choose low-stress days for your fasting. Don’t schedule a 24-hour fast on a day when you have a major presentation at work or an intense workout planned. Pick a quiet Sunday or a work-from-home day. Set yourself up for success, not struggle.
Important: Water becomes crucial here. Drink plenty of water throughout the day. Also, add a pinch of regular salt to your water to replace electrolytes you’d normally get from food.
Extended Fasts (2+ Days): Proceed with Extreme Caution
Fasts lasting 48 hours, 72 hours, or longer are a completely different category. These should not be done casually or frequently.
- How often: Only a few times per year at most, and only under medical supervision. Think of these as occasional health resets, not regular practices.
- Why people do them: Extended fasts trigger deeper cellular cleanup processes and can create significant metabolic changes. Some people use them therapeutically for specific health conditions.
- The risks are real: When you fast for multiple days, you risk serious electrolyte imbalances, dangerously low blood pressure, and nutrient deficiencies. The refeeding process (how you start eating again) is equally important and can be dangerous if done incorrectly.
My strong recommendation: If you’re considering an extended fast, please work with a healthcare provider. These are not DIY projects.
Special Considerations: When Fasting Needs Extra Care

Your individual health situation completely changes the answer to how often you should fast. Here are some common conditions that require caution:
- If you have diabetes (especially Type 1 or take insulin): Fasting can cause dangerous blood sugar drops or ketoacidosis. Only attempt very gentle time-restricted eating under close medical supervision.
- If you have low blood pressure, fasting often drops it even further, leading to dizziness and fainting. Stick to 12-14-hour14-hour fasts at most and monitor how you feel.
- If you have a history of gout, Fasting temporarily raises uric acid levels, which can trigger painful gout flares. Avoid prolonged fasts.
- If you have a history of eating disorders, Fasting might not be appropriate for you. Please discuss this thoroughly with your healthcare team.
- If you’re on any medications: Many medications need to be taken with food, or their dosing may need to be adjusted when you change your eating pattern.
- If you’re pregnant or breastfeeding: This is not the time to experiment with fasting.
Finding Your Rhythm: Practical Next Steps
So how often should YOU fast? Here’s how to figure it out:
- Start simple: Begin with a 12-14-hour overnight fast (dinner to breakfast) for a few weeks and see how you feel.
- Listen to your body: Fasting should feel challenging but not miserable. If you’re extremely irritable, dizzy, or struggling to function, you’re pushing too hard.
- Be consistent: It’s better to do a moderate fast regularly than to swing between extreme fasting and normal eating.
- Talk to your doctor, especially if you have any health conditions or take medications. We can help you find a safe, effective approach.
- Adjust as needed: Your fasting schedule might change with the seasons, your stress levels, your activity level, or your life circumstances. That’s completely normal.
Bottom Line
Fasting can be a powerful tool for health when done thoughtfully. For most people, daily time-restricted eating (like 16:8) done most days of the week is the sweet spot. It’s sustainable, safe, and effective.
Remember, the goal isn’t to fast as much as humanly possible. The goal is to find a pattern that enhances your health without dominating your life or damaging your relationship with food.
Start slow, stay safe, and make it work for your real life.
Medical Disclaimer
This article is for educational purposes only and does not replace personalized medical advice. Before starting any fasting regimen, especially if you have health conditions or take medications, consult with your healthcare provider. Fasting isn’t right for everyone, and what’s safe for one person may not be safe for another.
References
- Patterson, R. E., & Sears, D. D. (2017). Metabolic Effects of Intermittent Fasting. Annual Review of Nutrition.
- Longo, V. D., & Panda, S. (2016). Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan. Cell Metabolism.
- Longo, V. D. (2018). The role of fasting in the prevention and treatment of diabetes. Journal of Functional Foods.
- Tinsley, G. M., & La Bounty, P. M. (2015). Effects of intermittent fasting on body composition and clinical health markers in humans. Nutrition Reviews.
- Heilbronn, L. K., et al. (2005). Alternate-day fasting in nonobese subjects: effects on body weight, body composition, and energy metabolism. The American Journal of Clinical Nutrition.
- Barnosky, A. R., et al. (2014). Intermittent fasting vs. daily caloric restriction for type 2 diabetes prevention: a review of human trials. Translational Research.
- de Cabo, R., & Mattson, M. P. (2019). Effects of Intermittent Fasting on Health, Aging, and Disease. The New England Journal of Medicine.