As a medical professional, I frequently prescribe mupirocin ointment, often recognized by the brand name Bactroban. It is a powerful, topical antibiotic used specifically to treat bacterial skin infections. Mupirocin works by preventing bacteria from growing and spreading, making it an essential tool for conditions ranging from simple cuts that have become infected to serious bacterial skin diseases.
Because it is an antibiotic, using mupirocin correctly is crucial for two reasons: first, to ensure the infection clears completely, and second, to help prevent the development of antibiotic resistance. We’ll discuss exactly what it treats, the proper way to apply it, and the few side effects you should be aware of.
What is Mupirocin and How Does it Work?
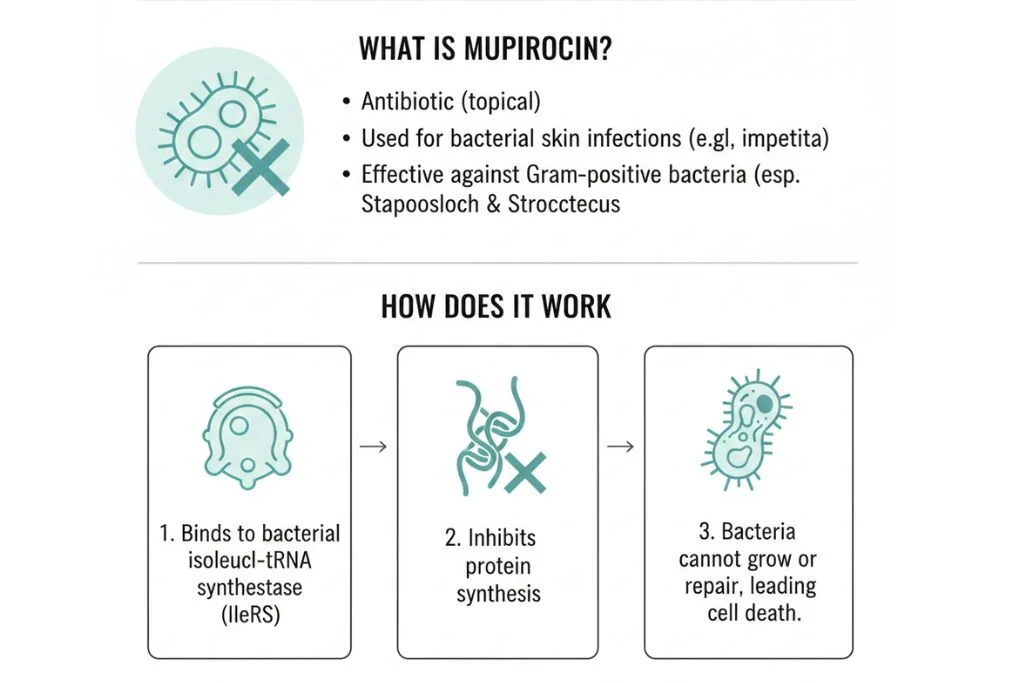
Mupirocin is a unique, naturally derived antibiotic that is only effective when applied to the skin (topically). It is not absorbed well into the body, which minimizes systemic side effects but concentrates its powerful action right where it is needed.
- Targeting Protein Synthesis: Mupirocin works by targeting a specific enzyme within bacterial cells called isoleucyl transfer RNA synthetase. This enzyme is essential for the bacteria to synthesize the proteins needed for growth and survival.
- The Result: By inhibiting this enzyme, mupirocin essentially halts the bacteria’s ability to build essential proteins, causing the bacterial cell to stop growing and eventually die. This makes it a bacteriostatic (stops growth) and, at high enough concentrations, a bactericidal (kills the bacteria) agent.
- Effective Against Staph: It is highly effective against Gram-positive bacteria, particularly Staphylococcus aureus (including MRSA) and Streptococcus pyogenes, which are the most common causes of skin infections.
Primary Uses and Therapeutic Benefits
Mupirocin is mainly used for localized skin infections and bacterial colonization.
- Impetigo: This is a very common use. Impetigo is a highly contagious skin infection, typically seen in children, characterized by red sores that quickly form crusty, yellowish scabs. Mupirocin applied directly to the lesions is highly effective.
- Folliculitis and Minor Skin Infections: It treats small infections around hair follicles and minor localized bacterial skin infections.
- Nasal MRSA Decolonization: Mupirocin comes in a specific formulation for use inside the nostrils. Many people carry methicillin-resistant Staphylococcus aureus (MRSA) bacteria in their noses without symptoms. Treating the nasal passage with mupirocin for a short course can eradicate this colonization, which is vital before certain surgeries or for people with recurrent infections.
- Clinical Insight: I had a patient with chronic, recurring boils. We tested him and found he was a nasal carrier of MRSA. A single course of nasal mupirocin stopped the recurring boils completely, showing the importance of eliminating the bacteria’s reservoir.
Application Instructions and Dosage Schedules
Using mupirocin correctly is critical for successful treatment. Do not simply rub it in; follow these specific steps.
- Hand Hygiene: Wash your hands thoroughly before and after applying the ointment.
- Clean the Area: Gently wash the infected area with soap and water, and pat it dry.
- Apply Sparingly: Apply a small amount of ointment to the affected area. You only need a thin film to cover the entire infected lesion. Do not use excessive amounts.
- Covering (Optional): You may cover the treated area with sterile gauze if your doctor recommends it, or if you need to protect the area from clothing.
- Schedule: The standard course is usually three times a day (TID) for 5 to 10 days. Follow your doctor’s exact instructions on the duration.
Key Dosage Schedule Example
| Condition | Frequency | Typical Duration |
| Impetigo | Three times a day (TID) | 5 to 7 days |
| Nasal MRSA | Twice a day (BID) | 5 days |
Export to Sheets
Practical Risks and Common Side Effects
Mupirocin is topical, so most side effects are localized and generally minor.
- Localized Reactions: The most common side effects are mild burning, stinging, itching, or pain at the application site. This is usually transient and does not require stopping the medication.
- Rash or Allergic Reaction: If you develop a widespread rash, swelling, or severe blistering, stop using the ointment immediately and contact your doctor.
- Secondary Infection: Rarely, the elimination of one type of bacteria can allow for the overgrowth of non susceptible organisms, such as a fungal infection (yeast). If the treated area worsens or develops white patches, consult your doctor.
- Avoid Eyes and Mouth: Mupirocin is meant for external use only. If you use it near the mouth or eyes, it can cause irritation. The polyethylene glycol base in some formulations can be harmful if applied to large open wounds or burns, especially in patients with kidney failure, due to systemic absorption.
Mupirocin and Antibiotic Resistance
As with any antibiotic, the single biggest long-term risk of misuse is the development of bacterial resistance.
- Preventing Resistance: Mupirocin resistance, particularly in Staphylococcus species, has been documented. To minimize this risk:
- Do not use it unnecessarily: Never use it for viral or fungal infections, only bacterial ones.
- Use the full course: Stopping early leaves stronger bacteria alive to develop resistance.
- Do not share: The prescription is for your infection only.
- Focus on Hygiene: Good hygiene (washing cuts thoroughly) is the first line of defense. Use mupirocin only when a bacterial infection is confirmed or highly suspected.
When to See a Doctor
While minor localized reactions are expected, see your doctor if:
- No Improvement: The infection shows no signs of improvement after 3 to 5 days of treatment.
- Worsening Symptoms: The area becomes larger, hotter, more painful, or you develop a fever.
- Severe Diarrhea: This is very rare with topical mupirocin but could indicate a systemic issue if the drug were ingested.
- Signs of Allergy: Difficulty breathing or swallowing, or a severe generalized rash.
Improvement Timeline
It is helpful to know what to look for when tracking the progress of a skin infection treated with mupirocin.
| Time Frame | Expected Observation | What to Look For |
| Days 1–2 | Reduction in oozing or weeping of the lesion. | Less redness/inflammation around the borders of the infection. |
| Days 3–5 | The sores begin to dry out and scab over. | Scabs should begin to flatten; pain should decrease significantly. |
| Day 7 (End of Course) | The skin should be healed or nearly healed, with only fading marks left. | Discontinue use only after the full course is completed, even if cleared early. |
Final
Mupirocin ointment is a valuable, targeted tool for fighting specific skin infections. By following the correct application steps, completing the full course of treatment, and using it only as directed, you ensure a complete recovery and play a role in slowing down the spread of antibiotic resistance. If you have recurrent skin infections, discuss the nasal decolonization strategy with your physician.
References
- U.S. Food and Drug Administration (FDA). (2022). Mupirocin ointment prescribing information.
- Chambers, H. F. (2018). The changing epidemiology of Staphylococcus aureus. Emerging Infectious Diseases.
- Konkobo, Y. S., et al. (2016). Mupirocin: a unique topical antibiotic. Journal of Dermatology and Clinical Research.
- Levin, J. M., & Saiman, L. (2018). Decolonization strategies for preventing methicillin-resistant Staphylococcus aureus infection. Current Opinion in Infectious Diseases.
- Spellberg, B., & Shlaes, D. (2011). The end of antibiotics and the need for new development models. Journal of Antimicrobial Chemotherapy.
- Corey, G. R., et al. (2019). Clinical experience with mupirocin for the treatment of impetigo. Pediatric Infectious Disease Journal.
- Livermore, D. M. (2009). Mupirocin resistance: a cause for concern. Journal of Antimicrobial Chemotherapy.

