When starting a medication like semaglutide (often prescribed for type 2 diabetes and weight management), it is common to experience changes in appetite, digestion, and energy levels. While the medication is highly effective, modifying your diet is crucial for minimizing potential side effects like nausea or constipation, supporting stable blood sugar, and achieving the best possible health outcomes. This guide offers practical, evidence-based nutritional strategies to help you navigate this transition successfully.
Core Principles of Eating on Semaglutide
Semaglutide works by mimicking a hormone that regulates appetite and insulin, causing a feeling of fullness and slowing down stomach emptying. This mechanism is beneficial but requires a shift in how and what you eat to prevent discomfort. Focus on smaller, nutrient-dense meals that are easy to digest.
1. Prioritize Protein at Every Meal
Protein is essential because it is highly satiating and helps preserve muscle mass, which can otherwise be lost during rapid weight loss. Aim for a small portion of lean protein first.
| Protein Source | Serving Size Example | Benefit |
| Lean Poultry | 3-4 oz (deck of cards) | Low-fat, complete amino acids |
| Greek Yogurt | 1 container (5-6 oz) | Probiotics aid digestion |
| Fish/Seafood | 3-4 oz | Omega-3 fatty acids |
| Tofu/Lentils | 1/2 cup cooked | Fiber-rich plant-based option |
2. Adopt Complex Carbohydrates (The Slow Burn)
Avoid large, refined carbohydrate meals (like big bowls of pasta or white bread), which can quickly fill the slowed stomach and lead to discomfort or blood sugar spikes. Choose smaller portions of complex carbohydrates for sustained energy.
- Good Choices: Oatmeal, quinoa, brown rice, whole-grain bread (in small amounts), sweet potatoes.
- Avoid/Limit: Large portions of white bread, sugary cereals, highly processed snacks, large servings of starchy vegetables (unless blended).
3. Mind Your Fats: Go Lean and Healthy
High-fat, greasy meals are often the most difficult to digest when stomach emptying is slowed, dramatically increasing the risk of nausea, acid reflux, and diarrhea.
Practical Tip: Replace fried foods with baked, grilled, or air-fried versions. Swap creamy sauces for vinaigrettes or herb-based sauces.
Simple Fat Hierarchy
| Fat Type | Example | Impact on Digestion (Semaglutide) |
| Healthy, Unsaturated | Avocado, olive oil, nuts | Generally well-tolerated (in moderation) |
| Saturated/Processed | Bacon, butter, whole milk | Can slow digestion further; increase discomfort |
| Fried/Greasy | Deep-fried chicken, french fries | Highest risk of severe nausea/reflux |
Managing Common Side Effects with Diet
The gastrointestinal (GI) system is often most affected by semaglutide. Strategic food choices can mitigate the discomfort.
A. Nausea and Vomiting
Nausea is the most common side effect, often peaking after the dose is initiated or increased.
- Eat Bland Foods: Follow the BRAT-plus diet (Bananas, Rice, Applesauce, Toast, plus broth and low-fat crackers).
- Stay Hydrated: Sip on clear liquids, electrolyte solutions, or ginger tea. Avoid drinking large amounts during meals.
- The “Smaller, More Frequent” Rule: Instead of three large meals, try five or six small mini-meals throughout the day.
Meal Frequency Diagram (Small vs. Large Meals)
| Traditional Approach | Semaglutide Approach |
|---|---|
| Meal 1 (Large) | Mini-Meal A (Small) |
| Meal 2 (Large) | Mini-Meal B (Small) |
| Meal 3 (Large) | Mini-Meal C (Small) |
| Mini-Meal D (Small) | |
| Mini-Meal E (Small) |
B. Constipation and Diarrhea
Constipation is frequent due to reduced food intake and slower motility. Diarrhea can also occur, often triggered by high-fat foods.
Step-by-Step for Constipation Relief:
- Hydration: Drink at least 64 ounces of water daily.
- Soluble Fiber Focus: Gradually increase soluble fiber (oats, apples, beans).
- Physical Activity: Gentle walking stimulates GI movement.
- Magnesium: Consider a magnesium supplement (check with your doctor).
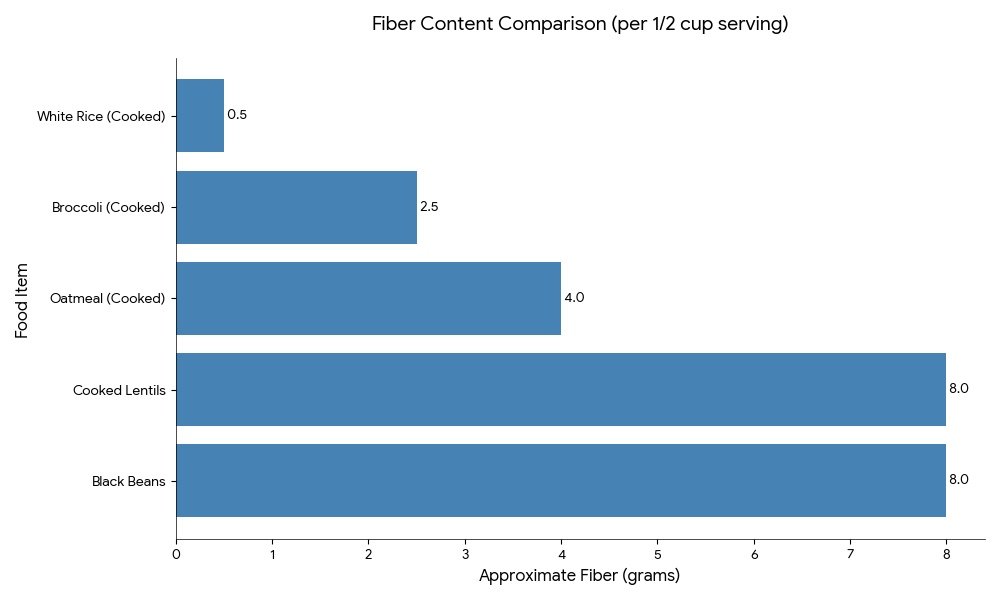
Fiber Content Comparison (per 1/2 cup serving)
| Food Item | Approximate Fiber (grams) |
| Black Beans | 8 |
| Cooked Lentils | 8 |
| Oatmeal (Cooked) | 4 |
| Broccoli (Cooked) | 2.5 |
| White Rice (Cooked) | 0.5 |
Lifestyle and Eating Habits
Optimizing results goes beyond just what you eat; it involves how and when you eat.
1. Mindful Eating Practice
Since you feel full faster, you must pay close attention to your body’s signals to avoid overeating, which leads to severe discomfort.
- Stop: Put your fork down after every few bites.
- Chew: Chew food thoroughly (aim for 20-30 chews per bite).
- Assess: Ask yourself: “Am I still hungry, or am I just finishing my plate?”
- Stop Eating: Stop the moment the sensation of fullness hits, even if food is left.
2. Hydration Strategies
Dehydration is a risk. Reduced appetite means fewer liquid-rich foods are consumed, and nausea can make drinking difficult.
- Keep a water bottle with you at all times.
- Infuse water with lemon, cucumber, or mint to make it more palatable.
- Swap sugary drinks (sodas, juices) for unsweetened tea or sparkling water.
3. Alcohol and Sugary Beverages
Alcohol can irritate the GI lining and contribute to dehydration. Sugary drinks offer empty calories that counteract weight goals. Limit or eliminate both.
When to See a Doctor
While mild GI symptoms are expected, certain signs warrant prompt medical attention:
- Persistent Vomiting: If you cannot keep liquids down for more than 24 hours.
- Severe Abdominal Pain: Intense pain, especially radiating to the back, which could indicate pancreatitis (a rare but serious risk).
- Signs of Dehydration: Dizziness, fainting, or significantly decreased urination.
- Persistent Low Blood Sugar (Hypoglycemia): Shaking, sweating, confusion (especially if you are also taking insulin or sulfonylureas).
Improvement Timeline
Dietary changes and the body’s adjustment to semaglutide take time.
| Time Frame | Expected Feeling/Symptom | Dietary Focus |
| Weeks 1-4 (Initial Dose) | Highest risk of nausea/GI upset. Strong appetite suppression. | Bland, high-protein liquids/soft solids. Prioritize hydration. |
| Weeks 4-12 (Dose Escalation) | GI symptoms lessen but may return with dose increases. Appetite stable, weight loss accelerates. | Reintroduce complex carbs. Monitor fat intake carefully. Increase fiber slowly. |
| Beyond 12 Weeks (Maintenance) | Symptoms minimal or gone. Sustained appetite control. | Balanced diet (protein, healthy fats, complex carbs). Focus on long-term nutritional sustainability. |
Final Advice
Semaglutide is a powerful tool, not a miracle cure. Your long-term success hinges on coupling the medication with sustainable lifestyle changes. View this time as an opportunity to reset your relationship with food: focus on quality over quantity, prioritize nutrient density, and listen carefully to your body’s new signals of fullness and satisfaction.
Medical Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition or treatment, and before undertaking a new healthcare regimen.
References
- American Diabetes Association. (2024). Standards of Medical Care in Diabetes.
- Gastrointestinal Society of Canada. (2023). Diet and Semaglutide Treatment.
- Wilding, J. P. H., et al. (2021). Once-Weekly Semaglutide in Adults with Overweight or Obesity. New England Journal of Medicine, 384(11), 989-1002.

