Noticing changes in your legs, hips, or arms can be confusing and stressful. Many women see their skin start to look dimpled, lumpy, or heavy and immediately think it’s cellulite. Diet and exercise are often blamed.
But here’s the truth: not all fat or uneven skin is the same.
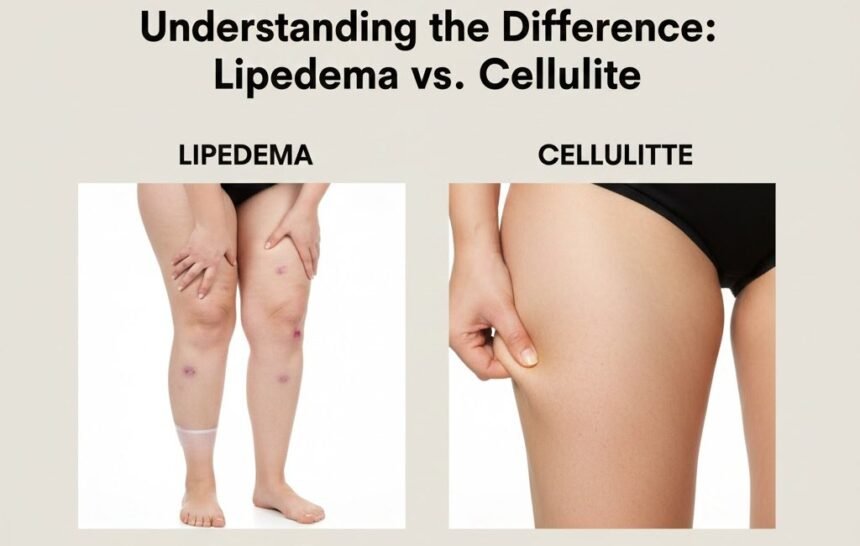
Lipedema is a chronic medical condition that affects fat distribution and can be painful, while cellulite is a harmless cosmetic change. Understanding the difference is the first step toward proper management and relief.
Why This Matters
I have spoken to dozens of women who spent years blaming themselves for stubborn leg fat. One woman shared:
“I was told to just work out harder or eat less. I followed every fitness plan, but my legs only got more painful, never smaller. I finally found out it was lipedema. That knowledge changed everything.”
Unfortunately, many doctors and websites lump lipedema with cellulite, which leads to misdiagnosis and frustration.
What Is Cellulite?
Cellulite is a cosmetic skin condition, not a disease.
It happens when fat pushes against connective tissue under the skin, creating a dimpled or “orange peel” appearance.
Key facts about cellulite
- Affects up to 90% of post-pubertal women
- Can occur at any weight, even in athletes
- Most noticeable on thighs, hips, buttocks, and sometimes arms
- Not painful
- Does not involve swelling, bruising, or tenderness
Example: A friend of mine is a marathon runner and has visibly dimpled thighs. She has perfect muscle tone, exercises daily, and has low body fat. The cellulite is purely cosmetic and does not affect her health.
What Is Lipedema?
Lipedema is a chronic fat disorder that causes abnormal fat accumulation, usually in the legs, hips, and sometimes arms. It almost always affects women.
How lipedema is different
- Fat is painful or tender
- Easy bruising occurs, even with minor bumps
- Fat is symmetrically distributed (both legs, sometimes both arms)
- Feet and hands are usually spared (cuff sign)
- Resistant to diet and exercise
Many women describe their legs feeling heavy or tight by the end of the day. Some even report sensitivity when touched.
Story:
A patient shared that after giving birth, her upper body slimmed down while her legs grew heavier and more painful. For years, she blamed postpartum weight gain. Proper diagnosis of lipedema allowed her to use compression therapy, which reduced pain and improved mobility.
Lipedema vs. Cellulite: A Quick Comparison
FeatureLipedemaCellulite
Pain: Yes, constant or tender. No
Bruising Easy and frequent , not typical
Distribution Symmetrical, hips to ankles/wrists. Usually, thighs/buttocks can be uneven.
Feet and hands Spared (cuff sign) Not affected
Swelling Common, worse later in the day Rare
Response to diet : Fat resistant; torso may lose weight . May slightly improve with fat loss
Medical condition Yes No
Signs and Symptoms of Lipedema
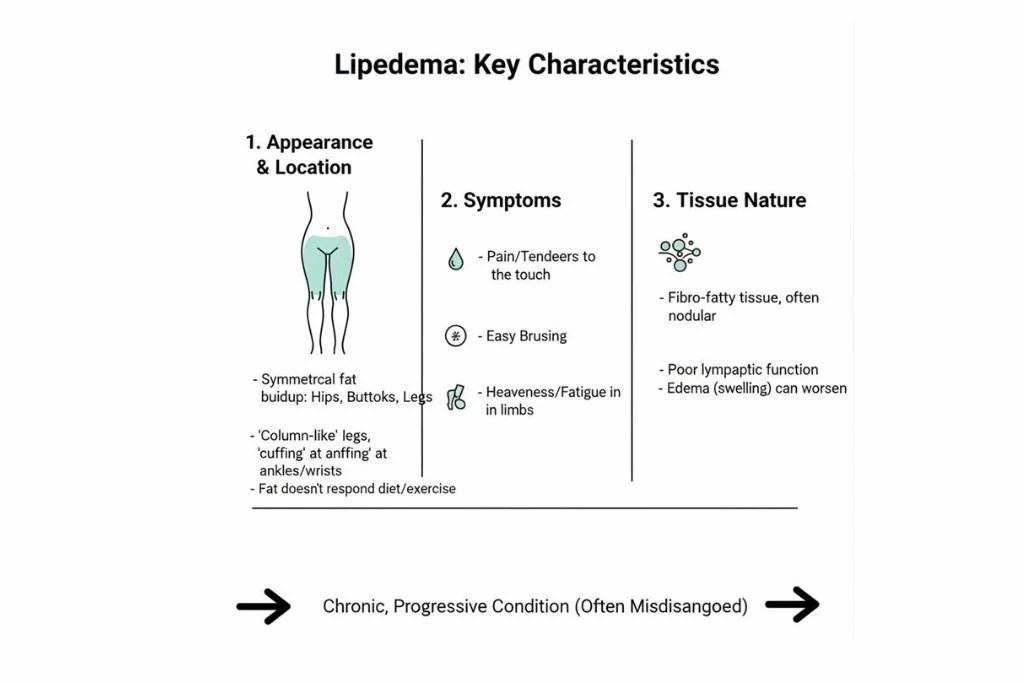
It is important to know what to look for beyond appearance.
Common symptoms
- Legs or arms feel heavy or tight
- Pain when walking, standing, or touching the fat
- Fat deposits that do not shrink with diet or exercise
- Easy bruising
- Swelling that worsens by evening or in warm weather
- Skin may feel soft, rubbery, or lumpy
Expert insight: Dr Emilie Foldi, a lymphology specialist, notes that many women with lipedema are unaware of the pain until it becomes chronic. Awareness is critical for early intervention.
Stages of Lipedema
Lipedema progresses gradually. Understanding the stages helps guide treatment.
| Stage | Appearance | Fat Characteristics | Symptoms |
|---|---|---|---|
| 1 | Skin smooth | Soft fat | Tenderness may start |
| 2 | Skin uneven/dimpled | Nodules or lumps form | Pain, bruising |
| 3 | Large fat lobules | Harder fat | Limb enlargement, swelling |
| 4 | Lipolymphedema | Fat and fluid combine | Swelling extends to feet |
Early detection is essential to prevent progression to stage 3 or 4, which can impact mobility and quality of life.
How Lipedema Feels
Pain and tenderness are key differentiators. Women often describe:
- A constant ache in the legs or arms
- Legs feeling heavy, tight, or stiff
- Discomfort during exercise
- Sensitivity to touch
This contrasts with cellulite, which causes no pain, only a cosmetic change.
Causes and Risk Factors
The exact cause of lipedema is not fully known, but several factors are linked:
- Hormonal changes (puberty, pregnancy, menopause)
- Genetics (family history is common)
- Microvascular fragility, which can lead to easy bruising
- Inflammation in fat tissue
Cellulite, in contrast, is mostly influenced by genetics, connective tissue structure, and fat distribution, without systemic inflammation or pain.
Can You Have Both?
Yes. Many women have both lipedema and cellulite. The key difference is still pain, bruising, and swelling. Understanding this can help tailor treatment appropriately.
Diagnosis
A proper diagnosis is often missed. Key tools include:
- Physical examination by a physician familiar with lipedema
- Assessment of symmetry, tenderness, and cuff sign
- Ruling out lymphedema (Stemmer’s sign)
- Imaging, such as ultrasound or MRI, in complex cases
Lipedema Management
While there is no cure, symptoms can be managed. Early treatment reduces progression and pain.
Compression Therapy
- Custom-fitted garments reduce pain and swelling
- Essential for daily support
Manual Lymphatic Drainage (MLD)
- Performed by certified therapists
- Helps move lymph fluid and reduce swelling
Exercise
- Low-impact activities are best:
- Swimming
- Water aerobics
- Cycling
- Walking
- Avoid high-impact exercise that worsens pain
Skin Care
- Moisturize daily
- Protect against injury
- Prevent infections (cellulitis)
Diet
While diet won’t reduce lipedema fat, an anti-inflammatory diet can help manage symptoms.
- Focus on whole foods, lean proteins, healthy fats, and colourful vegetables
- Limit sugar, refined carbs, and excess salt
Living With Lipedema: Tips
- Track your symptoms
- Keep a journal of pain, swelling, and activity tolerance. It helps your doctor adjust treatment.
- Choose the right clothing
- Compression garments can be uncomfortable at first. Try different fabrics and styles to find the best fit.
- Exercise with support
- Water workouts can reduce pressure on joints and limbs.
- Build a support network
- Online groups and communities help with emotional support and tips.
- Accept professional help
- Certified lymphedema therapists, vascular specialists, or lymphologists can provide treatment plans that really work.
Emotional Impact
Many women with lipedema experience guilt, frustration, or anxiety due to misunderstanding. Recognising it as a medical condition helps reduce self-blame and allows focus on effective management.
Frequently Asked Questions
Q: Can men get lipedema?
A: It is very rare but possible. Almost all cases occur in women.
Q: Can lipedema be cured?
A: Currently, there is no cure. Treatment focuses on symptom management and slowing progression.
Q: Will weight loss help?
A: Fat in affected areas is resistant. Weight loss may reduce fat in the upper body but not in the legs or arms.
Q: How do I know if I have lipedema or cellulite?
A: Pain, tenderness, easy bruising, symmetrical fat distribution, and resistance to diet/exercise are strong indicators of lipedema.
When to See a Doctor
Seek a medical professional if you notice:
- Pain or tenderness without injury
- Disproportionate fat distribution
- Easy bruising on legs or arms
- Swelling that worsens throughout the day
- Family history of similar symptoms
Early intervention prevents worsening and improves quality of life.
Final Thoughts
Cellulite is a cosmetic concern. Lipedema is a medical condition. Recognising the difference changes everything, from your self-perception to treatment strategy.
You are not lazy, overeating, or failing if diet and exercise don’t reduce leg fat. Proper diagnosis and support are the keys to comfort and mobility.
References
- Foldi, E., & Foldi, M. Foldi’s Textbook of Lymphology for Physicians and Lymphedema Therapists. Urban & Fischer, 2006
- Halk, A. B., & Damstra, R. J. First Dutch guidelines on lipedema using the international consensus on lipedema. Phlebology, 2017
- International Consensus Document. Best practice guidelines for the management of lipoedema. Wounds International, 2021