One of the most thrilling moments for expectant parents is hearing their baby’s heartbeat for the first time. It’s a profound reassurance and a deeply emotional milestone. Many wonder if a standard stethoscope, a familiar medical tool, can provide this precious sound at home. While the desire to connect with your baby in this way is completely understandable, the reality is that hearing a fetal heartbeat with a regular stethoscope is often challenging, if not impossible, until much later in pregnancy, if at all. This article will clarify why and explain the professional methods used for accurate detection.
Understanding Fetal Heartbeat Detection
Why a Standard Stethoscope Isn’t Ideal
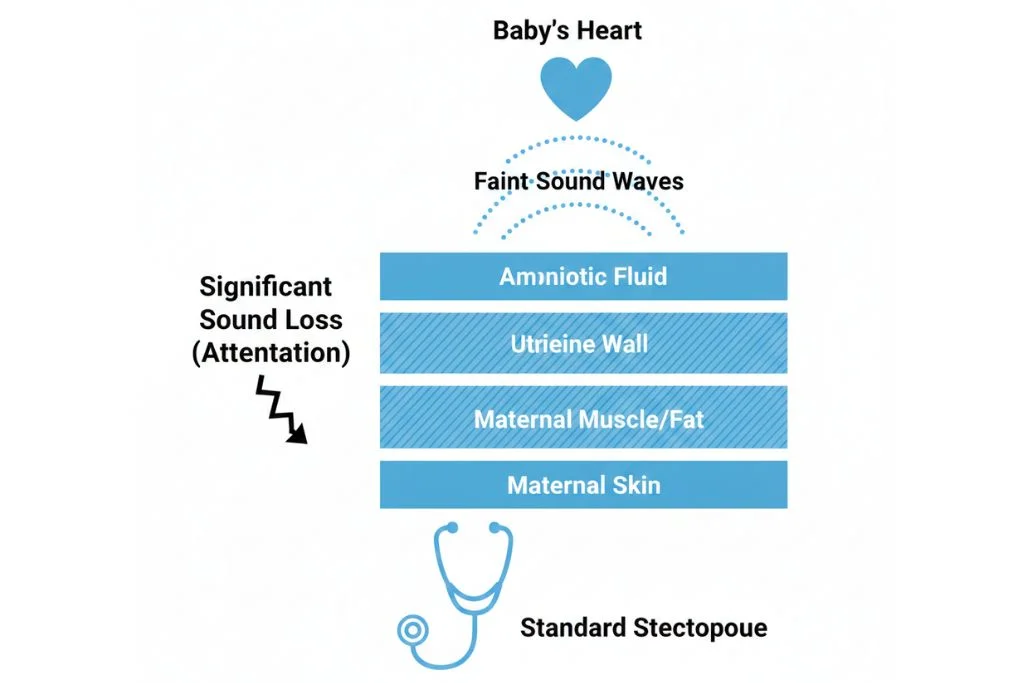
A conventional stethoscope is designed to amplify sounds close to the surface of the body, such as adult heart and lung sounds. A fetal heartbeat presents several unique challenges:
- Faint Sound: The baby’s heart is tiny, and the sound it produces is relatively faint, especially in early pregnancy.
- Maternal Tissue: The sound must travel through layers of maternal tissue (skin, fat, muscle, uterine wall, amniotic fluid) before reaching the surface of the abdomen. Each layer attenuates the sound.
- Background Noise: Internal maternal sounds, such as your own heartbeat, bowel sounds, and blood flow through the placenta, can easily mask the delicate fetal heartbeat.
- Fetal Position: The baby’s position in the womb can also make detection difficult, as the heart might be facing away from the abdominal wall.
Fetal Heart Rate vs. Maternal Heart Rate
It’s crucial to distinguish between the two. The normal fetal heart rate is significantly faster than an adult’s.
| Feature | Fetal Heart Rate | Maternal Heart Rate |
| Normal Range | 110−160 bpm (beats per minute) | 60−100 bpm |
| Sound Quality | Rapid, “whooshing” or “galloping” | Slower, “lub-dub” |
| Detection Method | Doppler ultrasound (professionally), specialized fetal stethoscopes | Standard stethoscope |
Professional Methods for Hearing the Heartbeat
Medical professionals use specialized tools designed to overcome the challenges of detecting a fetal heartbeat.
Doppler Ultrasound
The most common and effective method used in clinical settings.
- How it Works: A small handheld device (transducer) is placed on the mother’s abdomen, emitting high-frequency sound waves. These waves bounce off the baby’s heart, and the returning echoes are converted into an audible sound.
- Detection Timeline: A fetal heartbeat can typically be detected with a Doppler as early as 10−12 weeks of gestation, though sometimes earlier or later depending on the individual and equipment.
Fetoscope (Pinard Horn)
A specialized type of stethoscope used by midwives and doctors, particularly in later pregnancy.
- How it Works: This trumpet-shaped device is placed on the mother’s abdomen. The practitioner listens directly through the horn, using bone conduction to hear the magnified sounds.
- Detection Timeline: A fetoscope can usually detect a heartbeat reliably from 18−20 weeks of gestation onward, once the baby is larger and the heartbeat stronger. It requires skill and practice to use effectively.
ASCII Illustration: Sound Attenuation
Practical Guidance and Expectations
While home stethoscope use for fetal heartbeat detection has limitations, there are still ways to connect with your baby and monitor their well-being.
Step-by-Step for Home Listening (Later Pregnancy)
If you wish to attempt listening with a standard stethoscope, bear in mind it is most feasible in the third trimester (after 28 weeks), when the baby is larger and closer to the abdominal wall.
- Find a Quiet Room: Eliminate all background noise.
- Position Yourself: Lie down comfortably on your back (or slightly reclined) in a relaxed position.
- Locate the Baby: Gently feel your abdomen to try and determine your baby’s position. The heartbeat is often loudest over the baby’s back.
- Place the Stethoscope: Press the diaphragm firmly against your lower abdomen. Slowly move it around, listening intently.
- Listen Carefully: Differentiate between your own slower heartbeat and any faster, distinct “whooshing” or “galloping” sounds. This requires patience and often multiple attempts.
What to Listen For (and What NOT to Worry About)
- Your Own Heartbeat: This will be the most prominent sound. Don’t confuse it with the baby’s.
- Funic Souffle: Sometimes you might hear a “whooshing” sound of blood flowing through the umbilical cord. This is the same rate as the baby’s heart and is a good sign.
- Bowel Sounds: Gurgling noises are normal and unrelated to the baby’s heartbeat.
Beyond the Stethoscope: Other Ways to Connect
Relying on professional tools for fetal heart rate detection is safest and most accurate. However, there are many other wonderful ways to bond with your baby at home.
Bonding and Monitoring
- Feeling Movement: As your pregnancy progresses, you’ll begin to feel your baby move, kick, and even hiccup. This is a powerful and direct way to connect.
- Talking and Singing: Your baby can hear sounds from outside the womb from around 20 weeks. Talk, read, or sing to your bump.
- Prenatal Appointments: These are your most reliable source for monitoring your baby’s health, including heartbeat checks by your healthcare provider.
Avoiding Unnecessary Anxiety
- Home Dopplers: While home fetal Doppler devices are available, they are not recommended for routine home use without medical guidance. Misinterpreting sounds or failing to find a heartbeat can cause significant unnecessary anxiety for parents. Leave regular monitoring to the professionals.
Improvement Timeline
The ability to hear a fetal heartbeat progresses as the pregnancy advances and technology is applied.
| Period | Detection Likelihood (Stethoscope) | Detection Likelihood (Doppler) |
| Early Pregnancy (<10 weeks) | Extremely unlikely | Possible (6−8 weeks via transvaginal ultrasound, 8−10 weeks abdominally) |
| First Trimester (10−14 weeks) | Unlikely | High |
| Second Trimester (14−27 weeks) | Possible (late 2nd trimester) | Very High |
| Third Trimester (28−40 weeks) | More likely (but still challenging) | Very High |
When to See a Doctor
While home stethoscope listening is primarily for reassurance and bonding, it should never replace professional medical care. Contact your healthcare provider immediately if you experience:
- Reduced Fetal Movement: If your baby’s movements decrease significantly or stop, particularly after 28 weeks gestation.
- Vaginal Bleeding or Fluid Leakage: Any unusual discharge or bleeding.
- Severe Abdominal Pain or Cramping: Persistent or intense pain.
- Lack of Reassurance: If you are feeling anxious about your baby’s well-being for any reason, always contact your doctor or midwife.
Final Advice
Adopt the journey of pregnancy and the incredible bond you are forming with your baby. While a home stethoscope might offer a glimpse into your baby’s world later in pregnancy, it’s essential to rely on your healthcare provider for accurate and reliable monitoring of your baby’s heartbeat and overall health. Enjoy feeling those precious kicks and communicating with your little one in person!
Medical Disclaimer
This article is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding your pregnancy or medical condition.
References
- American College of Obstetricians and Gynecologists (ACOG). Fetal Movement Counts.
- Mayo Clinic. Fetal Heartbeat: When Can I Hear It?
- National Institutes of Health (NIH). Prenatal Care Fact Sheet.

