Deep, restorative sleep might be the new luxury. Would it be wishful thinking to expect silence in the middle of a war zone? Well, it’s a lot more deafening inside most people’s minds these days. That’s the interplay of sleep and stress at work.
A recent survey confirms this, as one-third of the 30,000+ respondents reported trouble falling asleep each night. Even among those who do fall asleep, they’re seldom able to secure the amount needed. The CDC shares that the amount of sleep an individual needs changes with age.
In reality, the most common rationalisation adults use for cutting back on sleep is stress. There is much truth to this, because modern life can be merciless at times. However, you cannot afford to neglect stress or sleep in light of their interplay.
This article will explore it in much detail, mainly through the lens of preventive wellness. It will go as far as presenting evidence-based strategies to break the cycle and optimise overall health.
Physiological Basis for Sleep and Stress Interaction

You must have heard the ‘cliche statement that sleep is the foundation of one’s health. On the other hand, stress triggers the body’s dreaded ‘fight or flight’ response. At a cursory glance, they seem to be in stark contrast, right?
Well, they are, but that doesn’t mean there’s no interplay between them. At the centre of it all, we have the body’s internal clock and the autonomic nervous system. Both systems are in constant dialogue.
This is precisely why one can affect the other, for better or for worse. If the interaction is negative, say, due to chronic stress, an individual experiences poor sleep. In turn, poor sleep tends to magnify one’s stress levels, and the cycle perpetuates.
Concrete Physiological Effects to Know
Let’s understand the relation between sleep and stress more closely, and also in a simplified way.
- Under intense stress, it gets challenging to fall asleep. This happens because the stress hormone cortisol keeps the brain awake. You may experience mental fatigue, but cannot fall asleep.
- Stress interrupts deep, restorative sleep. So, even if you do fall asleep on time, you’re not able to reach the deep sleep your body needs to repair tissues and strengthen immunity.
- This combination increases the body’s inflammatory response.
- It’s a vicious cycle because sleep deprivation heightens your brain’s sensitivity to stress. So, even minor concerns may seem overwhelming, thereby perpetuating the loop.
- If this goes on for a few weeks or even days, the brain struggles with focus and emotional regulation. The part controlling emotions (the amygdala) becomes reactive, and the part controlling decision-making (the prefrontal cortex) slacks off. You may experience anxiety at this stage or an overreaction to minor problems.
A 2024 analysis using mediation models found that stress not only coexists with poor sleep but actively worsens it. Rumination, emotion-focused coping, and smartphone dependence acted as the primary mediators.
So, the sleep-stress interaction indicates that preventive health must address both the mind and the body. Sleep hygiene should involve stress management, and stress management should involve sleep hygiene.
Health Consequences of Dysregulated Sleep and Stress Patterns
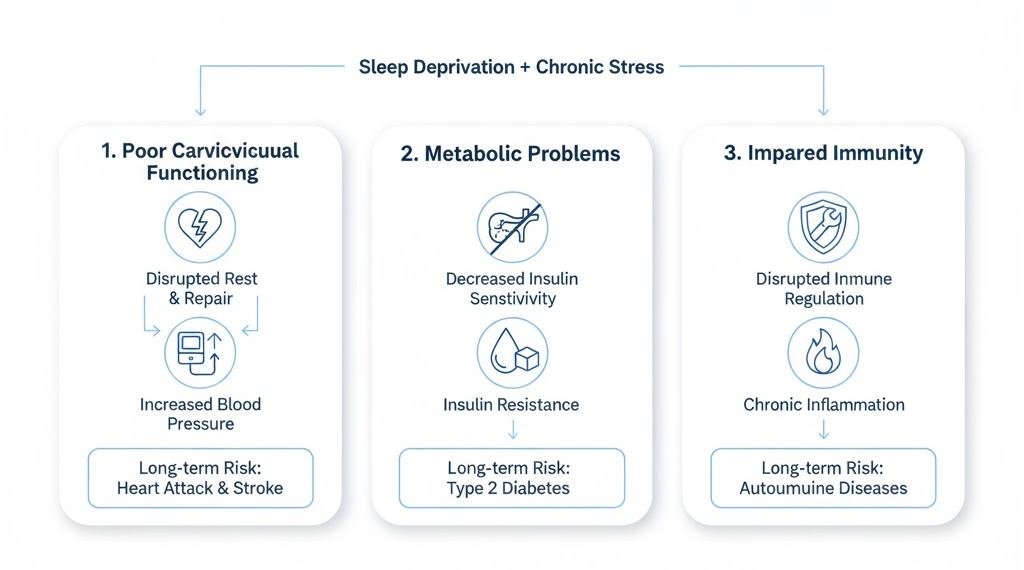
When the interplay between sleep and stress becomes negative, multiple systems suffer. Let’s look at the most important ones to understand why managing both matters for long-term health:
Poor Cardiovascular Functioning
As mentioned earlier, a lack of sound or deep sleep disrupts the body’s ‘rest and repair’ mechanism, which is usually active at night. This puts increased pressure on the blood vessels and the heart. A natural consequence is higher blood pressure.
In the long run, it rings alarm bells for adverse events, like heart attacks and strokes. In 2025, a study conducted on 9,641 adults aged 40 to 69 years confirmed this. It found that those with irregular sleep had significantly higher rates of all-cause deaths, including major cardiovascular events.
Those with healthy and regular sleep did not face such problems. This matters because even occasional nights of poor sleep, especially when combined with stress, can become a cardiovascular burden.
Metabolic Problems
The second significant danger of sleep deprivation combined with chronic stress is that it upsets metabolic regulation. In other words, your body’s insulin sensitivity will decrease. Insulin is the hormone that transports glucose from the blood into cells for energy production.
With disrupted insulin sensitivity, your cells won’t respond to the hormone efficiently. As a result, sugar and fat accumulate in the blood, a condition known as insulin resistance. Over time, it makes one susceptible to developing type 2 diabetes.
Again, studies back this up. A 2023 study of women aged 20 to 75 offered some interesting insights. Researchers found that restricting sleep to 6.2 hours or fewer per night for 6 weeks increased insulin resistance by 14.8%. Post-menopausal women were at greater risk, as their insulin resistance went as high as 20.1%.
Impaired Immunity
Sleep is essential for your body to repair and maintain itself. It will balance hormones, repair tissues, and regulate immune function/response. Inadequate or poor-quality sleep directly interferes with this vital process.
Gradually, the body’s inflammatory response increases. Now, inflammation in itself is not the problem. The human body needs acute inflammation, which is also its short-term response to injury or infection. That’s how the body takes action against anything harmful.
However, chronic inflammation begins to impair the immune system by constantly keeping it in ‘alert mode.’ That explains why those with insomnia are also prone to certain autoimmune diseases. Sadly, over 16% of the population worldwide is estimated to have insomnia.
Need for Better Sleep-Stress Evaluation in Preventive Care

The previous section discussed the three major areas that are affected by the negative interplay between sleep and stress. Those alone are enough to make the body vulnerable to a host of chronic illnesses and infections. For the longest time, preventive health has focused on measurable indicators, such as blood pressure, cholesterol, and body mass index.
These metrics are still important, but sleep quality and stress levels are equally important. Ignoring these two factors leads to a significant blind spot in preventive care. For effective integration of sleep and stress evaluation, preventive health strategies should:
- Examine sleep quality and duration: This would include looking out for short, fragmented sleep as well as daytime sleepiness. You must keep track of your bedtime routines, especially how well-rested you feel each morning.
- Monitor stress levels: Try identifying all the causes of ongoing stress in your life. Healthcare assessments should include perceived stress scores and health indicators, like cortisol regulation and heart rate.
- Incorporate behavioural and lifestyle interventions: mindfulness and relaxation techniques are essential. Such lifestyle interventions reduce stress while also enhancing restorative sleep.
- Identify early physiological changes: The body always gives signals when it’s struggling to cope with the effects of poor sleep and chronic stress. Even minuscule shifts in blood pressure or inflammatory markers should not be ignored. Preventive measures work best when issues are detected early.
The good news is that educational programs are also evolving to meet this growing need in clinical practice. Many are even allowing aspirants to enrolenrol in two complementary specialisation simultaneously, at their own pace, via online learning.
A dual online nurse practitioner program that enables students to pursue two advanced practice specialities simultaneously is a good example. As a result, practitioners gain a broader clinical perspective even as they learn.
Additionally, current academic and clinical training emphasise system-wide improvement strategies. As Rockhurst University puts it, issues in the evolving healthcare landscape can be analysed in light of quality and patient-safety initiatives.
Without comprehensive assessments that include sleep and stress metrics, improving patient outcomes is nearly impossible. When sleep-stress evaluation and interventions become central to preventive healthcare, patients may experience the following benefits:
- Reduced cardiovascular strain
- Improved metabolic balance
- Better immune system functioning
- Better cognitive and emotional resilience
Evidence-Based Strategies to Break the Vicious Cycle

So far, we have seen how chronic stress and poor sleep can feed off of each other. Fortunately, there are science-backed strategies that can help restore balance. Many of these strategies require simple lifestyle or behavioural changes. Applying them consistently will improve sleep, reduce stress, and ultimately, protect long-term health.
Synchronise Sleep With Natural Light Exposure
Natural light remains a major regulator of the human bio clock. In a recent study, researchers replaced the static lighting of a senior care facility with a dynamic lighting system. It mimicked the natural day-night light cycle. The results showed an impressive 43.4% improvement in sleep quality under dynamic lighting vs. the baseline.
Moreover, total sleep time increased by 3 hours 8 minutes, along with fewer nighttime awakenings. This means what you need is to align your sleep with your internal bio clock. Here are actionable tips to do so:
- Spend at least 10 to 30 minutes outside, even on overcast days.
- If daily exposure to natural light is not possible, consider dynamic indoor lighting that mimics the natural light-night cycle.
- Avoid using devices right before sleep. If necessary, then ensure the ‘night mode’ is on.
Align Daily Routines With Your Biological Clock
Believe it or not, there is a time to sleep and a time to wake up. Lately, there have been several debates on the significance of chronotype sleep. It refers to sleeping in alignment with one’s chronotype or the body’s natural tendency to sleep early or late. In simpler terms, this is in defence of both early risers and late sleepers.
Now, a recent study found that the timing of sleep and wakefulness matters a lot. Staying awake late habitually is more closely linked to mental health risks, including depression and mood instability. The point is that the human body has a natural ‘biological night,’ a time window when restorative sleep is most achievable.
Try not to miss that window, or you will become more vulnerable to stress and mood disorders. Here’s what you can do:
- Aim for a reasonably early bedtime and a consistent waking time. Try to eliminate social pressures or commitments wherever possible.
- Focus on sleep regularity, which means sleeping and rising at a fixed time each day. It’s fine if you cannot do so some days, but never shift your sleep hours wildly.
- If professional or personal constraints keep you up late, limit your exposure to bright, blue screens. Also, avoid caffeine intake and any brain-stimulating activities.
- If possible, schedule demanding tasks and heavy meals earlier in the day. This will respect the body’s internal rhythm, thereby preventing sleep disruption.
Participate in Intentional Stress-Recovery Techniques
If you wish to get out of your negative sleep-stress cycle, you have to be intentional. Firstly, sleep itself is a powerful way to reduce stress. A 2025 study argues that post-stress sleep is effective in reducing anxiety and boosting long-term emotional stability.
The usual sleep hygiene techniques, like meditation and mindfulness, are a must. However, you can even turn sleep itself into a strategic move against stress. It can be done by sleeping or at least lying down to rest after stressful events. Don’t worry, this doesn’t imply you should go to sleep the moment something stressful happens.
What you must do is prioritise high-quality sleep within the same day or night rather than staying awake late ruminating. Let’s explore a few practical, actionable tips:
- Protect your next sleep episode by maintaining a consistent bedtime routine.
- Consider taking a quick restorative nap of 15-30 minutes, especially during stressful days.
- Avoid coping strategies that block restorative sleep, such as alcohol or excessive screen time.
- Use a gentle routine to shed stress, such as relaxed reading or baking.
To sum it up, it’s high time that healthcare shifts its focus from treating the consequences of chronic stress or poor sleep. Staying one step ahead is about elevating sleep health to the level of exercise/nutrition in clinical assessments and patient education.
After all, that’s the heart of preventive healthcare, right? Patients must expect their clinicians to ask questions about sleep and stress patterns, much as they would check a pulse or heart rate.
An awe-inspiring fact about the human body is that it always functions in ways that promote health. Sometimes, it’s less about what more you can do and more about allowing the body to return to its natural state. Yes, sleep deprivation and chronic stress are not a part of that natural state! Don’t fight biology, and disease prevention will become inevitable.
Final Recommendation
To break the destructive cycle between poor sleep and chronic stress, preventive wellness must take a proactive, integrated approach. Individuals, clinicians, and health systems should treat sleep quality as a vital sign—just as necessary as blood pressure or heart rate—and evaluate stress with the same seriousness as any physical risk factor. Building daily habits that protect circadian rhythms, reduce physiological arousal, and support emotional resilience can dramatically improve long-term health outcomes.
Ultimately, prevention is not about doing more—it’s about aligning with the body’s natural biology. When sleep supports stress recovery and stress management supports restorative sleep, the body can heal, regulate, and thrive. Making sleep and stress management a non-negotiable part of preventive care is one of the most potent health investments any person can make.
References
1. Centers for Disease Control and Prevention (CDC)
CDC. How Much Sleep Do I Need?
Topic: Sleep duration guidelines across age groups
Year: 2024
Publisher: U.S. Department of Health & Human Services
2. American Psychological Association (APA)
American Psychological Association. Stress Effects on the Body.
Topic: Physiological impact of chronic stress on cardiovascular, metabolic, and immune function
Year: 2023
3. National Institutes of Health (NIH) / National Center for Complementary and Integrative Health (NCCIH)
NCCIH. Relaxation Techniques for Health.
Topic: Evidence-based stress reduction strategies (mindfulness, breathing, relaxation)
Year: 2024
4. National Institute of Mental Health (NIMH)
NIMH. Chronic Illness and Mental Health.
Topic: Relationship between stress, sleep problems, emotional regulation, and mental health
Year: 2024
5. Sleep Foundation
Sleep Foundation. How Sleep Affects Stress.
Topic: Bidirectional relationship between stress and sleep; cycle of dysregulation
Year: 2023
Publisher: National Sleep Foundation

