Piles, also known as haemorrhoids, are a common and often uncomfortable condition caused by swollen blood vessels in the rectum and anus. The primary culprit in many cases is chronic straining during bowel movements, which is usually a direct result of constipation.
We can’t change the anatomy, but we can certainly change the consistency of your stool. By focusing on your diet, specifically increasing your intake of dietary fibre, you can soften your stool, make it easier to pass, and significantly reduce the pressure that causes piles to form or flare up. This article provides a clear, practical guide to using high-fibre foods as your first line of defense and management strategy.
Power of Fibre: Mechanism of Action
Dietary fibre is the indigestible part of plant foods. When consumed, it moves through your digestive system, performing two essential tasks that are critical for piles management:
- Bulking: Fibre absorbs water, adding significant bulk and weight to your stool. This bulk stimulates the natural muscle contractions (peristalsis) in your colon.
- Softening: The water absorbed by the fibre keeps the stool soft and pliable. A smooth, bulky stool moves smoothly and quickly, eliminating the need to strain.
This dual action ensures comfortable, regular, and complete bowel movements, reducing the pressure that can aggravate or cause haemorrhoids.
High-Fibre Food Lists for Daily Management
Fibre comes in two primary forms: soluble and insoluble, and you need a good mix of both. Soluble fibre dissolves in water and forms a gel (which aids softening), while insoluble fibre provides the necessary bulk.
Group 1: Excellent Sources of Soluble Fibre
These foods are particularly helpful for softening stool and improving transit time.
| Food Category | Recommended Choices | Serving Size (Approximate) |
| Grains | Oats (rolled or steel-cut), barley | 1/2 cup (cooked) |
| Legumes | Black beans, kidney beans, lentils | 1/2 cup (cooked) |
| Fruits | Apples (with skin), citrus fruits, pears, bananas | 1 medium piece |
| Vegetables | Brussels sprouts, sweet potatoes, carrots | 1/2 cup (cooked) |
Group 2: Excellent Sources of Insoluble Fibre
These foods add significant bulk and structure to the stool.
| Food Category | Recommended Choices | Serving Size (Approximate) |
| Grains | Whole wheat bread, brown rice, whole-grain pasta | 1 slice or 1/2 cup (cooked) |
| Nuts/Seeds | Almonds, walnuts, ground flaxseed, chia seeds | 1 oz or 1 tbsp |
| Vegetables | Leafy greens (spinach, kale), celery, green beans | 1 cup (raw) |
| Fruits | Berries (raspberries, blackberries), plums | 1/2 cup |
Fibre Intake: Recommended Goals
Most adults need approximately 25 to 35 grams of fibre per day. If you are currently consuming less, it is vital to increase your intake gradually over several weeks to avoid gas, bloating, and cramping.
Target Daily Fibre Goal
| Age/Group | Daily Fibre Target (Grams) |
| Adult Women (under 50) | ≈25 g |
| Adult Men (under 50) | ≈38 g |
| Adult Women (over 50) | ≈21 g |
| Adult Men (over 50) | ≈30 g |
Visual Aid: Example Fibre Score
| Food Item (1 Serving) | Fibre Content (g) |
| Apple (with skin) | 4 g |
| 1/2 cup Black Beans | 8 g |
| 1/2 cup Oatmeal | 5 g |
| 1 slice Whole Wheat Bread | 3 g |
| Total in Example | 20 g |
Hydration: Critical Partner to Fibre
Fibre alone cannot do the job; it requires water to function correctly. Without adequate hydration, high-fibre foods can actually worsen constipation by creating a hard, compact mass.
Simple Hydration Diagram
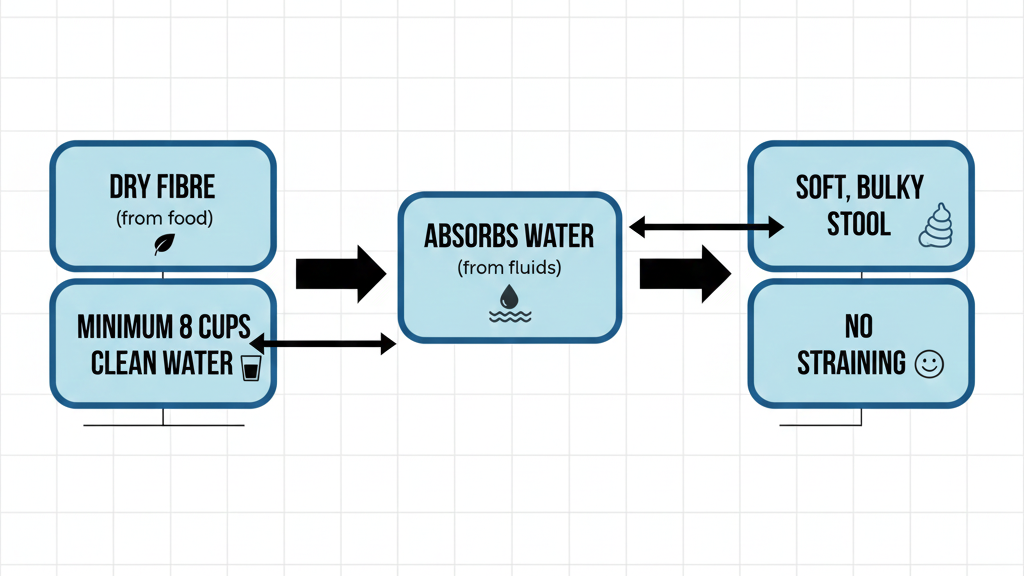
Practical Tip: Aim for 8-10 glasses (approximately 2-2.5 liters) of water daily. Increase this amount on days you consume particularly high-fibre foods like bran or supplements.
Lifestyle Adjustments for Lasting Relief
Dietary changes are most effective when paired with mindful lifestyle habits that support healthy bowel function.
Step-by-Step Stool Softening Plan
- Implement Gradual Fibre Increase: Add only 3-5 grams of fibre every 3-5 days. Start with a high-fibre breakfast (e.g., oatmeal with berries).
- Ensure Consistent Hydration: Keep a water bottle nearby and sip throughout the day. Avoid excessive caffeine or alcohol, which can be dehydrating.
- Establish a Routine: Attempt a bowel movement at the same time each day, ideally shortly after a meal (the gastrocolic reflex is strongest then).
- Use Proper Posture: Use a small footstool (in a squatting position) to elevate your knees above your hips. This naturally relaxes the puborectalis muscle, allowing for easier passage.
Expert Insight: Do not ignore the urge to go. Delaying a bowel movement allows more water to be absorbed, making the stool harder and initiating the cycle of straining and irritation.
When to See a Doctor
While dietary changes are highly effective for managing piles, certain symptoms require a medical evaluation to rule out other, more serious conditions and discuss treatment options.
- Persistent Bleeding: Any rectal bleeding, even if minor, should be investigated, especially if it changes in color or amount.
- Severe or Sudden Pain: Piles can cause discomfort, but severe, intense, or throbbing pain may indicate a thrombosed (clotted) haemorrhoid.
- Failure to Improve: If, after 6-8 weeks of dedicated high-fibre diet and hydration, your symptoms show no sign of improvement.
- Feeling of Incomplete Emptying: This can be a sign of a larger internal issue.
Improvement Timeline
Consistent dietary and lifestyle changes often yield noticeable results quickly, but full relief takes time as the body and the blood vessels heal.
| Phase | Duration | Expected Improvement |
| Initial Relief | 3 – 7 Days | Noticeably softer stool; less discomfort during bowel movements. |
| Symptom Reduction | 2 – 4 Weeks | Reduced frequency of painful episodes; decreased inflammation/swelling. |
| Sustained Management | 6 – 8 Weeks + | Regular, comfortable bowel habits established; minimal or no pile symptom |
Final Advice
The commitment to a high-fibre diet is not a temporary fix; it is a cornerstone of long-term digestive and rectal health. Think of fibre and water as a partnership: fibre does the bulking, and water does the softening. By consistently prioritizing plant-based foods and hydration, you can effectively manage and often prevent the discomfort associated with piles, leading to a significant improvement in your quality of life.
Medical Disclaimer
The information provided in this article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read here.
References
- American Gastroenterological Association (AGA) Guidelines for the Management of Haemorrhoids.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) resources on Constipation and Haemorrhoids.
- Position Paper of the Academy of Nutrition and Dietetics on the Health Implications of Dietary Fibre.

