Semaglutide has revolutionized medical weight-loss programs, offering significant clinical efficacy for patients managing obesity. However, its use requires a careful balance between achieving desired outcomes and maintaining patient safety. For healthcare providers, structured risk management and compliance practices are essential to mitigate potential adverse events, ensure regulatory adherence, and optimise patient outcomes. Understanding these elements is critical to implementing a semaglutide program that is both effective and safe.
Understanding Semaglutide and Clinical Implications
Semaglutide is a GLP-1 receptor agonist that helps regulate appetite and glucose metabolism. While its effectiveness is well-established, it is not suitable for all patients. Contraindications include a history of medullary thyroid carcinoma, pancreatitis, or severe gastrointestinal conditions.
Clinicians must have a thorough understanding of pharmacokinetics, dosing protocols, and patient-specific factors to ensure safe administration.
Completing specialized Semaglutide training equips healthcare providers with the knowledge needed to prescribe responsibly while minimizing risks.
Minimizing Risk from the Start
Effective risk management begins with comprehensive patient screening. Assessing medical history, current medications, comorbidities, and lifestyle factors is critical to identifying suitable candidates. Standardized screening tools, checklists, and clinical judgment help determine patient eligibility and reduce the likelihood of adverse events. Selecting patients who are motivated, informed, and have realistic expectations contributes to the overall success of semaglutide programs.
A Legal and Ethical Imperative
Informed consent is a cornerstone of patient-centered care and a key component of compliance. Patients must be fully aware of potential side effects, including nausea, vomiting, and gastrointestinal discomfort, as well as rare but serious risks such as pancreatitis or gallbladder disease.
- Clear communication about expected outcomes, adherence requirements, and treatment timelines builds trust and supports shared decision-making.
- Documenting these discussions meticulously ensures both patient protection and provider accountability.
Monitoring and Managing Side Effects
Despite careful screening, patients may still experience side effects. Implementing structured follow-up protocols, educating patients on warning signs, and providing strategies for managing mild adverse events are essential.
Establishing clear procedures for addressing severe reactions reinforces both safety and compliance. Utilizing risk management frameworks for weight-loss medications can help reduce liability while optimizing patient care.
Documentation and Compliance Best Practices

Accurate and thorough documentation underpins every aspect of risk management. Recording patient assessments, consent forms, dosing adjustments, and follow-up interactions is essential. Electronic health records (EHRs) can streamline this process, but providers must ensure compliance with HIPAA and other regulatory standards. Implementing a structured compliance program safeguards both patients and providers while promoting consistent, high-quality care.
Training and Continuing Education: Enhancing Provider Competence

Ongoing education and training are essential for providers prescribing semaglutide. Specialized programs offer comprehensive instruction on dosing strategies, patient counseling, adverse event recognition, and documentation protocols. Clinicians who complete such training are better equipped to manage complex cases, reduce errors, and maintain compliance with evolving guidelines.
Pharmacy Considerations and Prescribing Compliance
Collaboration with pharmacies is a key component of semaglutide programs, especially when compounded formulations are involved.
Providers must understand the regulatory framework surrounding compounding, dispensing, and prescribing to avoid compliance pitfalls.
Clear communication with pharmacists and adherence to both state and federal regulations are essential to maintain program integrity and ensure safe, compliant patient care.
Developing a Safe and Compliant Semaglutide Program
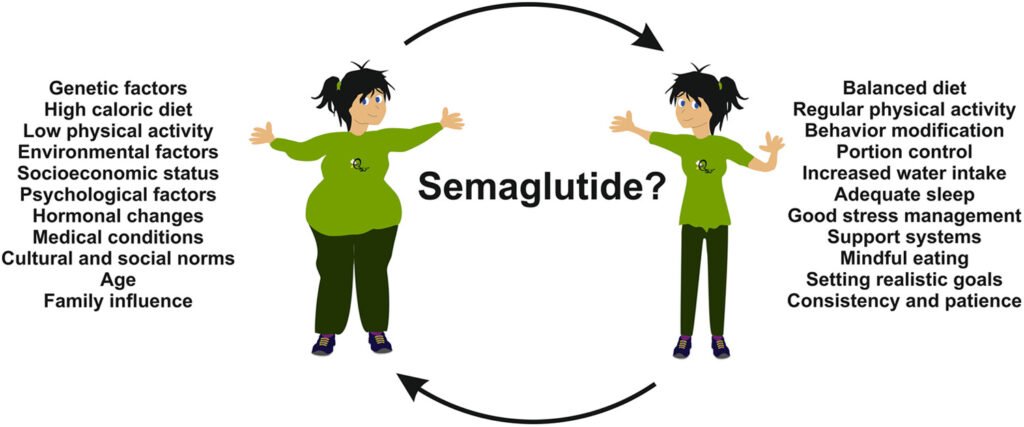
Implementing a semaglutide weight-loss program requires an integrated approach that prioritizes patient safety, regulatory compliance, and clinical efficacy. Structured screening, thorough informed consent, continuous monitoring, accurate documentation, and ongoing training are all essential components. By embedding these practices into routine care, providers can deliver patient-centered treatment while minimizing risk and liability.
Conclusion
Semaglutide offers significant clinical benefits in the management of obesity, but its use demands careful attention to risk and compliance. Providers who invest in structured Semaglutide Training, maintain robust documentation practices, and follow established risk management strategies are positioned to deliver safe, effective, and legally compliant care. By emphasizing patient selection, education, and monitoring, clinicians can optimize outcomes while fostering trust, accountability, and excellence in weight-loss therapy.

