Diphenhydramine is one of the most widely available medications on the market, commonly sold under brand names like Benadryl. It’s an antihistamine that many people use for everything from seasonal allergies to mild insomnia. Because it’s available over the counter and has been around for decades, patients often assume it is completely benign.
While diphenhydramine is very effective for short term use, its mechanism of action is complex and leads to several significant side effects that people often overlook, especially the strong sedating and anticholinergic effects. Understanding these effects is key to using it safely, particularly in older adults or when using it regularly for sleep.
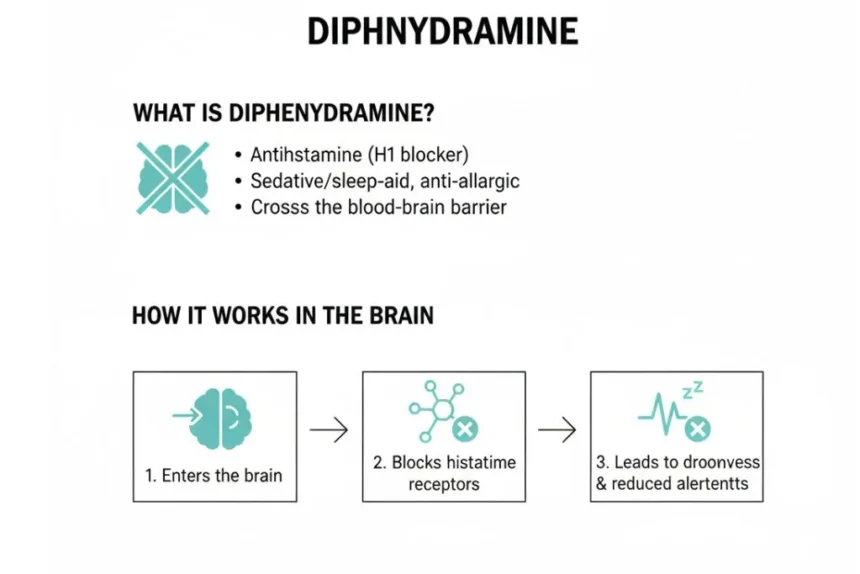
What is Diphenhydramine and How Does it Affect the Brain?
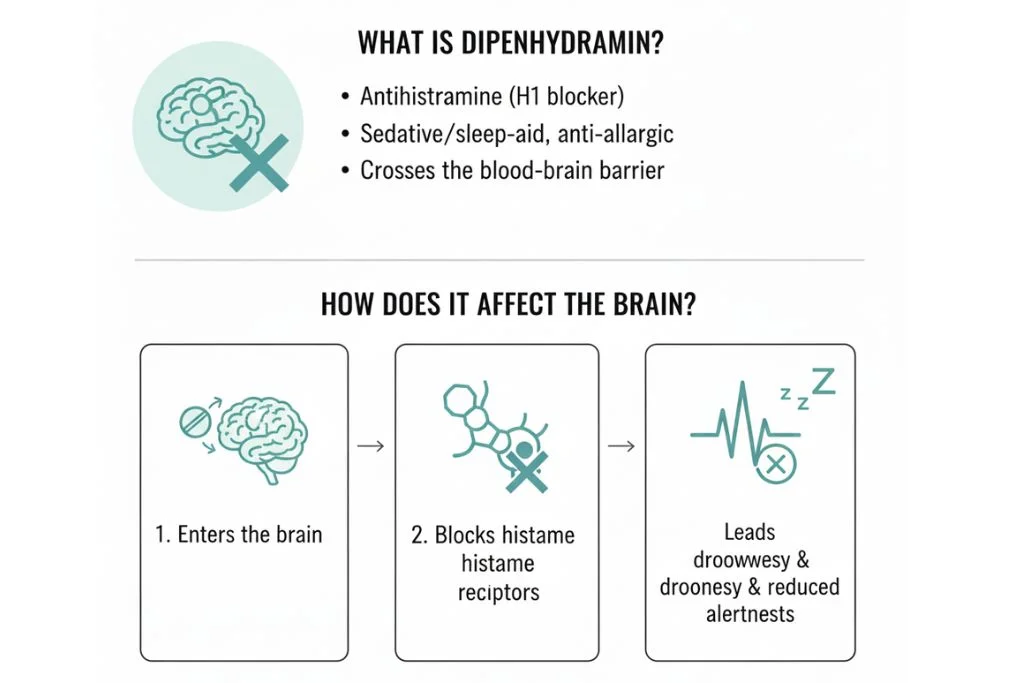
Diphenhydramine is a first-generation antihistamine with two primary mechanisms of action, both of which contribute to its noticeable effects.
Targeting Histamine:
Its primary role is to block histamine’s action by antagonizing the H₁ receptor. Histamine is released during allergic reactions and is responsible for symptoms such as itching, sneezing, and watery eyes. By blocking H₁ receptors, diphenhydramine effectively relieves these allergy symptoms.
Sedative Effect:
Unlike newer (second-generation) antihistamines, diphenhydramine readily crosses the blood–brain barrier. In the brain, it blocks central H₁ receptors, which play a key role in maintaining wakefulness. This central action leads to significant drowsiness and sedation, which is why diphenhydramine is commonly used as an over-the-counter sleep aid.
Anticholinergic Effect:
Diphenhydramine also blocks muscarinic acetylcholine receptors, which are essential for memory, muscle control, and regulation of bodily secretions. This anticholinergic activity accounts for many of its side effects, including dry mouth, blurred vision, constipation, urinary retention, and cognitive impairment—particularly in older adults.
Primary Uses and Therapeutic Benefits
Diphenhydramine is a versatile, fast acting medication used across several medical applications.
- Allergic Reactions: Highly effective for acute allergy symptoms such as runny nose, sneezing, hives, and itching.
- Insomnia (Temporary): Its strong sedating effect makes it useful for treating occasional difficulty falling asleep.
- Motion Sickness: It helps block signals in the brain related to nausea and vomiting caused by movement.
- Parkinsonian Symptoms (Off-Label): Due to its anticholinergic properties, it is sometimes used to help manage mild tremors and stiffness in patients with Parkinson’s disease or drug induced movement disorders.
Clinical Insight: I advise patients to keep a small supply of diphenhydramine only for acute situations, like a sudden allergic rash or a night when they are truly unable to sleep due to stress. It should be seen as a short term “break glass” solution, not a daily sleep routine.
Dosage Forms, Schedules, and Safe Use
Diphenhydramine is available in tablets, capsules, liquids, and topical creams. It is essential to choose the correct form and dose.
- Standard Dose: The typical adult dose is 25 mg to 50 mg, taken every 4 to 6 hours for allergies, or once at night for sleep.
- Avoid Combining Products: A major risk is accidental overdose. Many cold medicines (like Tylenol PM) already contain diphenhydramine. You must check labels carefully to avoid “double dipping” and taking more than the maximum daily limit (usually 300 mg).
- Do Not Drive: Given the strong sedative effect, never take diphenhydramine before driving, operating machinery, or performing any task requiring alertness. This impairment can last 8 hours or longer.
Medication Category Comparison
| Medication | Main Mechanism | Sedation Level | Risk for Older Adults |
|---|---|---|---|
| Diphenhydramine | Blocks H₁ histamine receptors and has strong anticholinergic effects | High | High (confusion, urinary retention, falls) |
| Cetirizine (Zyrtec) | Selective H₁ histamine receptor blockade | Low | Low |
Practical Risks and Common Side Effects
The anticholinergic effects of diphenhydramine are the cause of its most common side effects.
- Dry Mouth and Eyes: Reduced saliva and tear production is very common. This can lead to dental issues over time if used regularly.
- Drowsiness and Fatigue: While a benefit for sleep, daytime grogginess (hangover effect) is a major issue, often lasting well into the next morning.
- Constipation and Urinary Retention: Reduced muscle activity in the digestive and urinary tracts can lead to these problems, especially concerning for men with prostatic hypertrophy (enlarged prostate).
- Dizziness and Confusion: This is a particularly serious risk for older adults. The confusion (delirium) can mimic dementia and lead to dangerous falls.
Long Term Risks and Misuse Concerns
Regular use of diphenhydramine carries serious long term risks that people often underestimate.
- Tolerance and Rebound Insomnia: If you use it daily for sleep, you will quickly develop tolerance, meaning the 50 mg dose stops working. When you stop taking it, you often experience severe rebound insomnia, making your original sleep problem worse.
- Potential Cognitive Decline: Emerging research suggests that chronic, long term use of strong anticholinergic drugs like diphenhydramine is associated with an increased risk of cognitive decline and potentially dementia, particularly in the elderly population.
- Misuse for Sedation: Dependency can form when individuals rely on the drug to handle daily sleep anxiety, leading to a vicious cycle of tolerance and increased dosage.
When to See a Doctor
While diphenhydramine is available without a prescription, you should consult a doctor if:
- Insomnia Lasts Longer Than 2 Weeks: Chronic sleep issues require investigation into the underlying cause (stress, sleep apnea, RLS), not just masking with a sedative.
- Symptoms Worsen or Change: Your allergy symptoms do not improve, or you develop a severe, unusual reaction.
- Urinary Issues: You experience significant difficulty urinating while taking the medication.
Improvement Timeline
Diphenhydramine is fast acting. Its effects are usually felt very quickly, but this rapid action means it is unsuitable for chronic problems.
| Time Frame | Expected Observation | What to Monitor |
| 30 Minutes | Onset of sedative effect; relief from acute itching/sneezing. | Monitor for dizziness, especially when standing up. |
| 4–6 Hours | Peak effect time; drowsiness is strongest. | Avoid any activity requiring focused attention. |
| 8–12 Hours | Drug concentration drops; hangover effect may persist. | Assess morning alertness; if groggy, the dose may be too high. |
Final Advice
Diphenhydramine is an excellent tool for quick relief of acute allergy symptoms or very occasional sleeplessness. For chronic issues, however, it is a poor choice due to its strong side effects and potential for tolerance. For regular use, speak to your doctor about newer, non sedating antihistamines (like loratadine or fexofenadine) for allergies, or long term behavioral changes (CBT I) for sleep. Preserve the effectiveness of diphenhydramine by using it sparingly.
Medical Disclaimer
The information provided in this article is for informational purposes only and is not intended as medical advice, diagnosis, or treatment. It is not a substitute for professional medical care. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition, the use of over the counter medications (including starting, stopping, or managing side effects of diphenhydramine), or any chronic health issues.
References
- U.S. Food and Drug Administration (FDA). (2023). Diphenhydramine Monograph.
- Bramlage, P., et al. (2015). Anticholinergic load and risk of cognitive impairment in older adults. Current Alzheimer Research.
- Vitiello, M. V., et al. (2009). Treatment of chronic insomnia: an American Academy of Sleep Medicine review. Sleep.
- Church, M. K., & Church, D. S. (2018). Pharmacology of antihistamines. Indian Journal of Dermatology.
- Rudis, J., et al. (2019). The safety of first generation antihistamines in the elderly: A review of the evidence. Journal of Clinical Pharmacy and Therapeutics.
- National Sleep Foundation. (2020). Antihistamines as a Sleep Aid.
- Kuno, Y., et al. (2017). Anticholinergic burden and cognitive function. JAMA Internal Medicine.