If you’ve tried eliminating foods, taken probiotic supplements, read countless articles, and still feel bloated, exhausted, or have unpredictable digestion, you’re not failing. You’re likely dealing with a level of complexity that generic advice isn’t designed to address.
Digestive health sits at the intersection of your diet, stress levels, sleep quality, nervous system, genetics, and the trillions of microbes in your gut. When something goes wrong, pinning it down requires more than a symptom checklist or a popular elimination protocol.
This guide explains how practitioner-led, personalised gut care works, why it often succeeds where self-directed approaches haven’t, and what you can expect from a qualified gut health professional. The clinical approach of The Gut Guy naturopathy team is used as a working example of how thoughtful, evidence-based personalisation looks in practice.
Why Generic Gut Advice Often Falls Short
General health articles, apps, YouTube videos, and even well-meaning friends tend to offer population-level guidance: low-FODMAP diets, more fibre, less sugar, more probiotics. These are safe starting points, but they are averages, and you are not an average.
What Generic Advice Does Well
- Raises awareness of gut health basics
- Provides safe general starting points
- Encourages dietary improvement
- Works well for mild, uncomplicated symptoms
- Accessible and low-cost
Where It Consistently Fails
- Ignores underlying root causes
- One-size recommendations for unique biology
- No mechanism for tracking or adapting
- Misses connections between systems
- Can worsen symptoms if applied incorrectly
Important Awareness: Trying multiple diets, supplements, or protocols without professional guidance is extremely commonand extremely exhausting. Research shows that the frustration of trial-and-error approaches can worsen gut symptoms by increasing stress hormones and disrupting sleep. If you’re stuck in this cycle, it may be time for a different approach.
Same Symptoms, Very Different Causes
One of the most important things to understand about digestive health is that identical symptoms can have completely different origins. Treating symptoms rather than causes rarely produces lasting results.
Take bloating as an example. Most people assume it means they need to cut out bread or beans. But bloating can be caused by:
- Low Stomach Acid: Insufficient acid means food isn’t broken down properly before reaching the small intestine, leading to fermentation and gas production.
- Altered Gut Motility: Slow movement through your digestive tract gives bacteria more time to ferment food, which is often linked to nervous system function.
- Dysbiosis: An imbalance in your gut microbiome allows gas-producing bacteria to dominate.
- SIBO (Small Intestinal Bacterial Overgrowth): Causes fermentation to occur earlier in digestion, leading to bloating shortly after eating.
- Impaired Bile Flow: Low bile output reduces fat digestion, causing bloating and discomfort.
- Visceral Hypersensitivity: Heightened pain response in the gut makes normal gas feel intensely uncomfortable. This is neurological, not dietary.
The same principle applies to reflux, constipation, loose stools, and food intolerances. Each symptom can stem from a wide range of mechanisms, and treating only one while missing others often provides partial or no relief.
Clinical Insight: Experienced practitioners, like The Gut Guy naturopathy team, are trained to “read behind” symptoms, connecting what you feel to the physiological processes behind it rather than matching symptoms to a standard protocol.
What a Thorough Clinical Assessment Looks Like
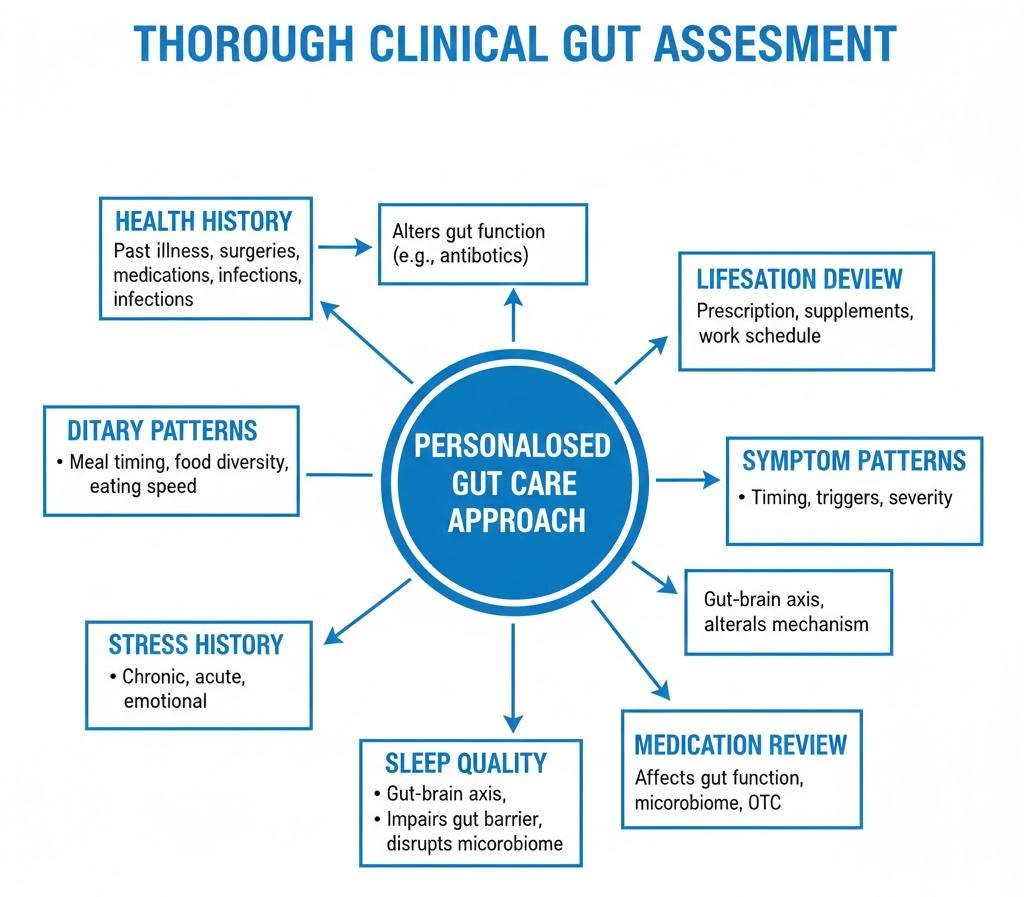
A personalised gut care approach begins before any treatment plan is written. A comprehensive assessment typically covers multiple layers of health because the gut does not exist in isolation.
| Assessment Area | What the Practitioner Looks For | Why It Matters |
|---|---|---|
| Health History | Past illnesses, surgeries, medications, infections | Events like gastroenteritis, antibiotic courses, or abdominal surgery can permanently alter gut function |
| Dietary Patterns | Meal timing, food diversity, eating speed, fluid intake | How you eat can be as important as what you eat |
| Stress History | Chronic, acute, emotional, or occupational stressors | The gut–brain axis means psychological stress directly alters gut motility and permeability |
| Sleep Quality | Duration, consistency, sleep disorders, shift work | Poor sleep impairs gut barrier function and disrupts the microbiome |
| Symptom Patterns | Timing, triggers, severity, what helps or worsens | Reveals mechanism—morning vs post-meal symptoms, predictable vs random |
| Lifestyle Demands | Activity levels, work schedule, social environment | Treatment must be realistic within your actual life |
| Medication Review | Prescription meds, supplements, OTC drugs | Many medications significantly affect gut function and microbiome composition |
Often, it’s the combination of factors, such as stressful periods, antibiotics, and a low-diversity diet, that explains why gut function changed at a specific point in time.
Gut Health Testing: What It Can and Cannot Tell You
Testing is increasingly popular in gut health care and can provide valuable data. But it’s important to understand what tests canand cannotreliably tell you.
Common Gut Health Tests
- Comprehensive Stool Analysis: Examines microbes, inflammatory markers, digestive enzyme output, and gut permeability indicators. Useful for identifying dysbiosis, infection, or poor digestion.
- Hydrogen/Methane Breath Tests: Diagnose SIBO and assess carbohydrate malabsorption; require careful interpretation due to false positives/negatives.
- Organic Acids Testing: Offers insight into metabolic function, mitochondrial health, and microbial metabolite production.
- Food Sensitivity Panels: IgG antibody tests are widely offered, but elimination-reintroduction remains the gold standard.
- Inflammatory Markers (Calprotectin, CRP): Distinguish between inflammatory bowel disease and functional gut disorders.
Critical Point About Testing: Test results are data points, not diagnoses. A practitioner interprets results in context, identifying clinically meaningful findings and integrating them into the broader clinical picture.
When Testing Adds Value:
- Symptoms haven’t responded to initial interventions
- Clinical picture suggests specific mechanisms
- Ruling out serious pathology is necessary
- Results will change the treatment strategy
- Interpreted by a qualified practitioner
When Testing May Not Help:
- Done without context or rationale
- Used as a first step before assessment
- Interpreted without guidance
- Results wouldn’t change the approach, leading to unnecessary food restrictions
Personalised Nutrition: Why One Diet Doesn’t Fit All
Nutrition is central to gut health, but no single diet works for everyone. Individual responses vary based on microbial composition, enzyme output, gut motility, inflammation, and genetics.
Problem with Rigid Dietary Protocols
- Protocols like low-FODMAP, GAPS, SCD, or carnivore can provide short-term relief.
- Risks when followed without guidance:
- Reduced microbial diversity over time
- Masking symptoms without addressing causes
- Nutritional deficiencies develop slowly
- Fear-based food restriction and disordered eating
- Prolonged unnecessary elimination
Practitioner Approach: Experienced clinicians start with minimal restriction, monitor response, and gradually expand dietary variety. The goal is nourishment and microbial diversity, not rigid exclusion.
What Personalised Nutrition Looks Like:
- Baseline dietary assessment
- Targeted modification of the smallest meaningful changes
- Structured symptom monitoring
- Systematic food reintroduction
- Long-term dietary diversification
Lifestyle, Stress & the Gut Brain Axis
The gut and brain communicate via the gut–brain axis, a network of nerves, hormones, and immune signals. This explains why stress, anxiety, grief, and poor sleep directly impact digestion.
How It Affects You Day to Day:
- Stress and Gut Motility: Can accelerate (diarrhoea) or slow (constipation) digestion
- Chronic Stress: Increases intestinal permeability
- Sleep Deprivation: Alters microbiome composition and gut barrier integrity
- Anxiety: Amplifies visceral pain signals
Realistic Lifestyle Adjustments:
- Eat without distractions
- Maintain regular meal times
- Prioritise sleep consistency
- Short post-meal movement
- Diaphragmatic breathing before meals
- Limit alcohol, especially with meals
How Practitioners Balance Evidence with Individual Needs
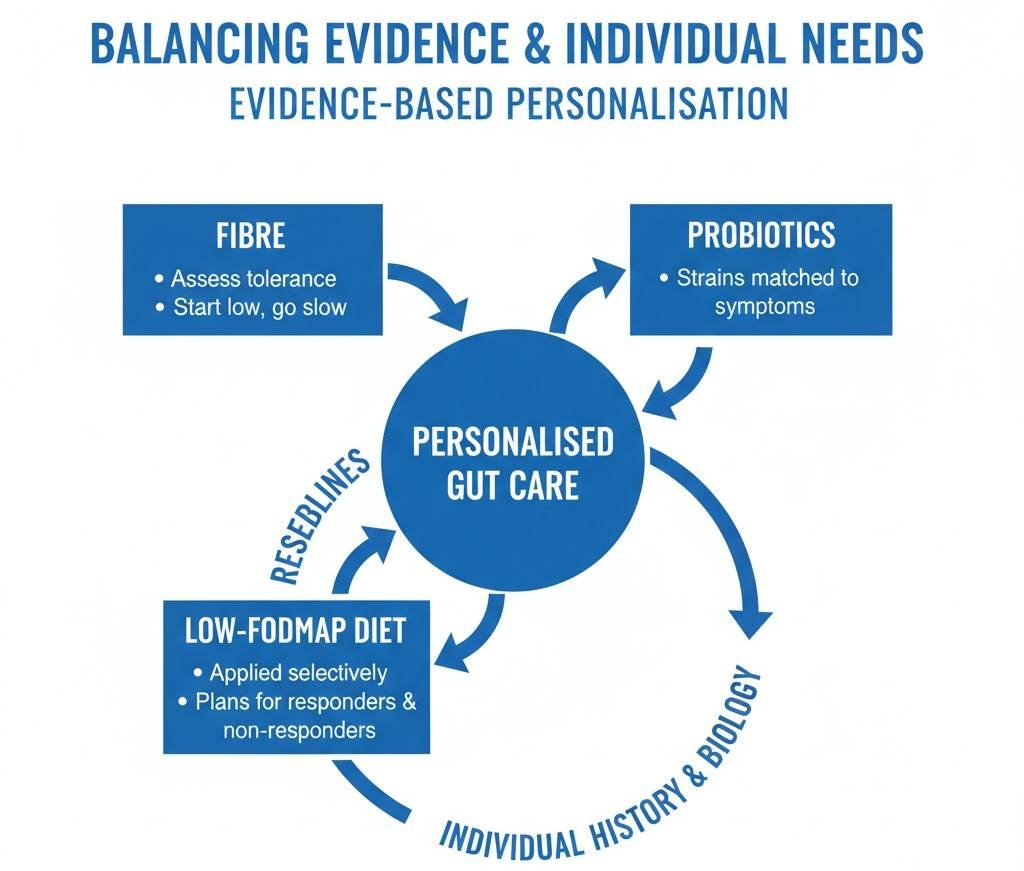
Personalised care is no less scientific than following standard protocols. Research provides averages; practitioners apply it to your unique history, biology, and goals.
Evidence-Based Personalisation:
- Fibre: Practitioners assess whether you can tolerate more without worsening symptoms
- Probiotics: Strains are matched to your symptoms
- Low-FODMAP: Applied selectively, with plans for both responders and non-responders
The Gut Guy naturopathy team integrates research with individualised treatment, reflecting true evidence-based care.
When to See a Gut Health Practitioner
Professional support is warranted if:
- Symptoms persist >8–12 weeks despite diet changes
- Multiple elimination diets have failed
- Symptoms impact quality of life
- Unpredictable flares unrelated to food
- Strong connection between stress and digestion
- Past gut infection, food poisoning, or antibiotics
- Feeling overwhelmed by conflicting information
- GP says “nothing is wrong,” but symptoms persist
See a GP or Emergency Services Immediately If You Experience:
- Blood in stools or black/tarry stools
- Unexplained weight loss
- Persistent vomiting
- Severe abdominal pain
- Symptoms waking you from sleep
- Family history of colorectal cancer with new bowel changes
Questions to Ask Your Gut Health Practitioner
- What qualifications and training do you have specifically in digestive health?
- Based on my history, what might be driving my symptoms?
- What does your treatment approach look like, and why for me specifically?
- How will we track progress, and what if this approach isn’t working?
- When would you refer me to a GP or gastroenterologist?
- What is a realistic timeline for improvement?
Final Thoughts
Gut health is deeply personal, shaped by your biology, history, and lifestyle. Generic advice often falls short because it doesn’t address root causes. A practitioner who considers the full picture, connects the dots, and builds a plan suited to your life can profoundly improve your digestive health.
The Gut Guy naturopathy team exemplifies personalised care that is evidence-based, responsive, and respectful of the complexity of individual gut health. Care should aim not just to manage symptoms, but to understand why they occur.
Medical Disclaimer
This guide is for educational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional before making dietary, supplement, or lifestyle changes. Seek immediate care for emergency symptoms.
References & Further Reading
Cryan, J.F. et al. (2019). The Microbiota-Gut-Brain Axis. Physiological Reviews, 99(4), 1877–2013. doi:10.1152/physrev. 00018.2018
Gibson, P.R. & Shepherd, S.J. (2010). Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. Journal of Gastroenterology and Hepatology, 25(2), 252–258.
NICE. (2017; updated 2023). Irritable bowel syndrome in adults: diagnosis and management. Clinical guideline [CG61]. nice.org.uk/guidance/cg61
Konturek, P.C. et al. (2011). Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. Journal of Physiology and Pharmacology, 62(6), 591–599.
NHS. (2024). Irritable bowel syndrome (IBS). nhs.uk/conditions/irritable-bowel-syndrome-ibs
Quigley, E.M.M. (2013). Gut Bacteria in Health and Disease. Gastroenterology & Hepatology, 9(9), 560–569.
Carabotti, M. et al. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology, 28(2), 203–209.
Markowiak, P. & Śliżewska, K. (2017). Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients, 9(9), 1021. doi:10.3390/nu9091021
British Dietetic Association. (2023). Food Fact Sheet: Irritable Bowel Syndrome. bda.uk.com
Rao, S.S.C. & Quigley, E.M.M. (2016). The use of breath tests in the diagnosis of small intestinal bacterial overgrowth. Current Gastroenterology Reports, 18(1), 3.
Guthrie, E. & Hamlin, P.J. (2020). The importance of psychological factors in the management of IBS. Frontline Gastroenterology, 11(4), 318–323.
Mental Health Foundation. (2024). Gut health and mental health. mentalhealth.org.uk

